Search the Community
Showing results for tags 'Paramedic'.
-
Hey guys I have a question on how to become a flight nurse. So I already have an EMT background completed. I tried to apply for a bachelor in Nursing but I didn’t get in. And now I don’t know what to do. There is a school near me to become an RN and there’s another school that offers the paramedic program. Which route do you guys recommend I take? I also have the other option of trying to apply again to the school of bachelor in nursing but it will take a year until I find out if I get in or not. What do you all suggest I do? Should I wait to hear back from that school again or should I go for paramedic or just get my RN then do a bridge to paramedic to be a flight nurse?
-
Hello Everyone, I am a civilian Critical Care Paramedic with a question for our Military Medic brothers and sisters. Do you feel your military medical training is aqueduct to operate as a Paramedic in the civilian population? This has been a long standing question I have had. I have worked with many military medics who are frustrated by the limited role they are given when transitioning to civilian EMS. I do share the thought that military medic are underutilized in the civilian setting when only being given an EMT level certification. That being said, it has always been my belief that military medical training if not sufficient to prepare someone to care for the vastly different and more diverse medical issues, situations and populations in the civilian world. I have never been through a military medic training course, so what I am seeking is insight to what is covered in the course. I am hoping to either confirm my beliefs or to learn new information that would give me a different point of view and a better perspective on the depth of military medical training. Lastly, I do believe a bridge program should be set up for military medics to help them quickly obtain paramedic status in the civilian world. The program should take the knowledge and skills learned from the military training and add in training on pediatrics, geriatrics, OB and any other areas not covered. All I ask is some insight from those that have gone through military medic training and especially those that have made the transition to civilian Paramedic. Thank you for your selfless service to our country.
-
There has been a lot of chatter on social media regarding a degree requirement for Paramedics to be eligible for certification. What are your thoughts on this?
-
Lifestar Chicago is hiring Flight Paramedics! APPLY ONLINE AT https://bit.ly/2BJjgKV Job Details Description Responsible for providing high quality pre-hospital advanced life support including assessment, triage, and treatment utilizing standards and guidelines established by Air Methods Community Based Services (CBS) Medical Director(s). You’ll be responsible for carrying out the mission and goals of Air Methods CBS assuring that safety remains the highest priority throughout the transport continuum. Essential Functions and Responsibilities: Provides pre-hospital advanced life support care from the initial contact until patient care is relinquished to the accepting medical facility; maintains thorough patient care documentation. Practices within his/her scope of practice as defined by the states regulating each base and Air Methods CBS. Maintains competency in knowledge and psychomotor skills by participating in ongoing laboratory and clinical experiences. Communicates educational needs to the Medical Base Supervisor and Medical Education Coordinator. Maintains documentation of required licensure, certifications, continuing education, aviation and safety training, OSHA and HIPAA training, clinical rotations, and advanced procedures. Attends minimum of six educational programs per year pertinent to his/her practice. Knowledgeable in use and routine maintenance of all equipment and supplies used by Air Methods CBS. Responsible for reporting medical equipment failures and taking initial steps to insure repair of equipment as directed. Maintains adequate supplies onboard aircraft to deliver patient care. Keeps aircraft clean and orderly to insure rapid response to all transport requests. Participates in patient and referring institution follow-up and planned outreach marketing and education activities. Functions as a medical flight member by attending pre-mission briefings and mission debriefings and completes necessary documentation. Assists in pre-mission liftoff checklist and assists pilot as requested, i.e., radio, navigational, and visual observation activities. Complies with safety standards to assure safety of self, medical personnel, patient, and equipment. Conducts aircraft safety briefings as needed. Serves as a flight resource to neonatal/pediatric personnel when transporting specialty patients by helicopter. Performs advanced skills and procedures as approved by Air Methods CBS Medical Director(s). Serves as a role model, educator and clinical resource. Participates regularly in departmental activities, projects and committees (to include research and publishing opportunities). Maintains awareness of current issues related to pre-hospital care through participation in professional activities, i.e., national, state legislative--elected or appointed. Other Duties as assigned. Education & Experience High school diploma or general education degree (GED) and at least three years’ related experience and/or training; or equivalent combination of education and experience Minimum three (3) years’ recent experience in a busy 911 system Previous critical care transport and flight experience preferred Skills Skills as required to practice as a paramedic as defined by assigned state scope of practice and advanced practice skills as defined by Medical Director(s) and Medical Standards. Maintains positive interpersonal relationships with colleagues, EMS representatives, hospitals and the public while executing strong interpersonal skills and a high degree of collaboration at all levels Demonstrates high critical thinking and reasoning skills and strong attention to detail while working in a fast paced environment that requires ability to prioritize and multi-task Ability to work a flexible schedule including 24 hour shifts, overtime, and an on-call rotation Dependable and self-motivated while working in a frequently changing environment. Excellent communication and presentation skills, both written and verbal Computer Skills Proficient with Microsoft Suite, including Word, Excel, PowerPoint and Outlook Certificates, Licenses, Registrations Registered EMT-P licensed in state(s) served National Certification may be required to meet state licensure requirements Specialty certification: (FP-C or CCP-C) required within two (2) years of hire Current certifications in Healthcare Provider BLS/CPR; ACLS; PALS or equivalent (AHA courses if state or county required) and advanced provider ITLS or PHTLS (if state or country required) Advance trauma course: one (1) of the following is acceptable: TNCC, ATLS/ATCN, TNATC or CAMTS-approved advanced trauma course prior ro completion of third-rider status (Please note advanced skills lab must accompany all of the above mentioned advanced trauma courses) NRP certification prior ro completion of third-rider status NIMS Training IS 100, 200, 700, 800 and HazMat upon hire Air Methods is an EEO/AA employer. Qualified applicants will receive consideration for employment without regard to race, color, religion, sex, sexual orientation, gender identity, national origin, disability or protected veteran status. Qualifications Education Required High School or better. Licenses & Certifications Required Drivers License Equal Opportunity Employer/Protected Veterans/Individuals with Disabilities The contractor will not discharge or in any other manner discriminate against employees or applicants because they have inquired about, discussed, or disclosed their own pay or the pay of another employee or applicant. However, employees who have access to the compensation information of other employees or applicants as a part of their essential job functions cannot disclose the pay of other employees or applicants to individuals who do not otherwise have access to compensation information, unless the disclosure is (a) in response to a formal complaint or charge, (b) in furtherance of an investigation, proceeding, hearing, or action, including an investigation conducted by the employer, or (c) consistent with the contractor’s legal duty to furnish information.
-
I'm an EMT Student trying to decide what path to follow. I know for a fact that I want to do EMS, and nothing else, but the best paying jobs in my area are for FF/EMT-P. There are ambulance districts around me, but pretty much all but one pays less than $15 an hour. I really don't have any desire to go putting on turnout gear and climbing up ladders, but I have heard that many firefighters are on the ambulance majority, if not all the time. I wouldn't even mind doing medical calls on the fire truck and extrications. The FD jobs are very hard to get, but is it worth it? I don't want to be stuck on a fire truck all of the time.. Should I just stick to EMS? Thanks, JT
- 17 replies
-
- 3
-

-
- firefighter
- paramedic
-
(and 1 more)
Tagged with:
-
This post is for all of your potential EMT's PAramedic's who are discouraged because you have taken the test and didn't make it. I have been an Iowa Paramedic for 10 years, outside the state of Iowa I am an I-99. I have taken the NREMT Paramedic test 13 times total. I was to the point of that if I didn't pass before 3/31/18 I would lose my paramedic and go down to an AEMT losing half of my skills. I had tried everything you can think of I used Medic skills, EMT test prep, bought practice books for the test. Bought a book from the school that I got my BS degree in that was for the NREMT. My next to the last attempt was in Jan and failed. I studied contact Distance CME to enroll in their NREMT test prep program. I then scheduled the test for this past weekend. I tested on Sat. 17th. I didn't realize that I was testing on a holiday weekend so I was resigned to the long wait of waiting till Tuesday morning. I went I tested was cut off at around 80-85 questions just over an hour into the test. I was unsure how I felt coming out of the test but I felt pretty good going as the Distance CME class prepared me for the exam, During the exam, I felt like I had seen the questions before and I was pretty confident on the answers for the most part. I just out of curiosity checked the results yesterday morning. I was surprised to see that the results said exam scored. So the panic of the previous attempts had started to creep in again. I clicked on the results and to my surprise and relief, I passed. I wrote this to tell all of you that there is hope no matter how many attempts you have tried. I would highly recommend the Distance CME NREMT test prep program they have EMT and Paramedic level programs. I can now rest a little easier knowing that I have taken and passed the exam. Although I am not NREMT P I am a PM instead of a IA-P.
-
Hello,I'm a student paramedic currently studying paramedic science at the University of East Anglia (in England). I was hoping that someone might be able to offer some information about the possibility of an ambulance placement in Scandinavia, Norway in particular? In my 3rd year, before qualifying I'll have the opportunity for an elective placement for about a month. I haven't admittedly been able to find much information on the ems system in Norway but I'm aware that it is staffed by paramedics and EMT's with similar qualifications to those in the UK. Any more information anyone might have to offer on the EMS system in norway would be really great, aswell as any information about the opportunity to shadow/experience in norway :)!Thanks for any help anyone might be able to offer :)!
-
1.)How old were you when you decided or thought about becoming a paramedic 2.) What was your college experience? 3.) How many years did it take to graduate? 4.) What could you give to someone going into the business? 5.) what is your American dream? 6.) is it achievable? 8.) if you could live your life all over again would you become a paramedic again? Why ke why not? 9.) Was this your first choice of a career? 10.) was there a time when you wanted to give up? If you answered these questions thank you so much. I'm writing a college and career essay and I'm interested in talking this as a job.
-
Hi guys! So I've noticed previous posts about this and have researched it for hours. Unfortunately most posts on here are rather old. I'm hoping some of you have new info! I'm currently a certified paramedic in Ontario and Alberta, looking into the process of moving to the US. Any kind of information (as current as possible) would be awesome! Thanks!
-
Hey everyone! Just thought I'd come back since I got a lot of positive/good advice last time I posted. I am currently on the downslide of EMT-B and looking for preparation advice about Medic school. I am pushing medic off till January to do A&P because I think it will help me a lot (I took Human Bio so I technically don't have to) with medic school. What other things should I prepare for/focus on while I'm in EMT-B and A&P? I've heard medic school is a nightmare.. Any class I should take beforehand? Or book I should buy?.. Etc
-
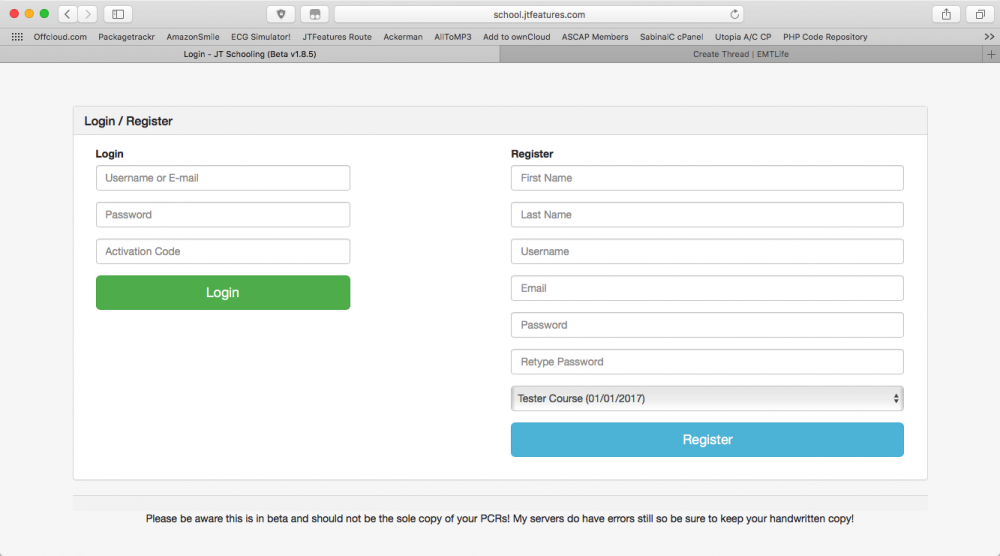
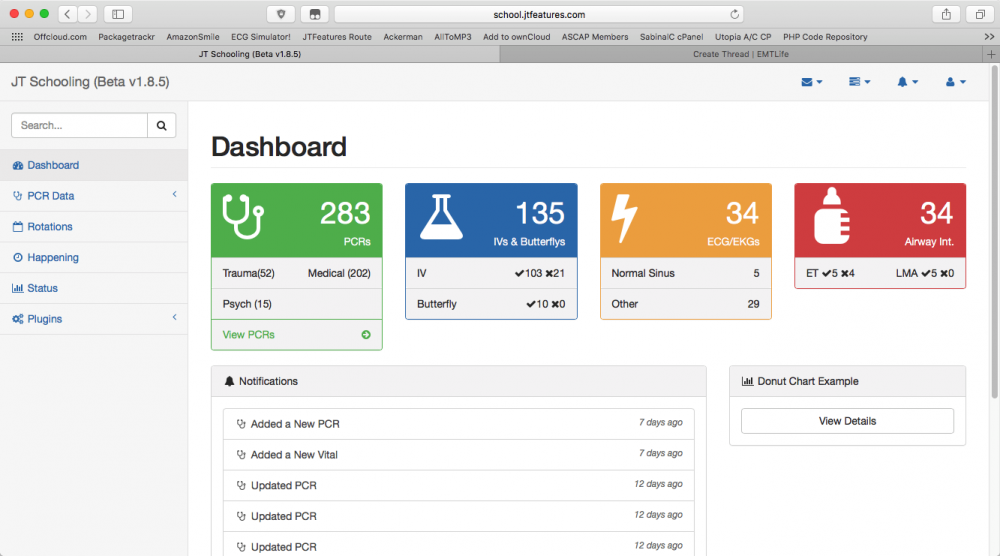
Hello all! I am new here but I have been reading threw the internet trying to find some help with something. I have been working on a program that I have been using over the last year to track my patient contacts as well as terms and stats on my training complete with reports to see when I would be cleared to take my test (as my school was constantly losing my stuff). So the more I worked with it and the more I learned about my needs as a paramedic student I decided that I should clean up the code and make a public version for my classmates. Well sadly they are not computer savvy and did not take the time to actually use it and so that idea failed. But I have continued to work with it and play with different ideas and I think it is something that could really help a LOT of other young students from EMT -> Paramedic (as ECAs do not have rideouts). I am attaching the public version and I would like to see what you all think. If its something that you would like to use yourself then by all means let me know and ill get you setup! I am working on a version 2 that has a new look and some new features but as I am still a student myself I don't have a lot of time to work on it. If some of you are coders and would like to talk about completing some additions/modifications to the project I would love to bring in some new people to the project as well (also really need help with bitbucket setup and running) I have also started work on a mobile app for the PCR side of the application to be used in the field as students to rideouts so iOS and android programmers are also needed. This is not a program I am charging for right now. If i have to charge in the future I will make a new area for schools to get custom features but I want to keep it free for the wonderful future medics like myself so they can have a little less worry and get those nice new patches! Public Version: school.jtfeatures.com
-
So being a senior in high school, I was wondering what courses and programs/clubs are a good bonus to have along with Bio and Physics for EMT as I want to go into Paramedic training. I already have First Responder Training which includes advanced first aid and BLS. I have partial access to the scope of practice for a MFR and I am also going into EMS cadets. I am not sure if I will get any extra training for EMS cadets but I do know I am allowed to go on ridealongs with the EMTs. Is there anything else that may make me more of a choice to be accepted into an EMT training course and further my training by going into a Paramedic course?
-
I'm a paramedic FTO and preceptor, I wrote this ebook and have been given out to my interns and new hires for the past year with great success they learnt the ebook like the back their hand and become great medics. If you want something that might assist you be a better, quicker and more efficient paramedic check this out. Spread the word! https://bit.ly/29Em0cv - Link modified so that a portion of the money spent on the book will benifit EMT City. - Admin
-
Hey, I wanted to know, if I get qualified as a Paramedic in Israel, if I came back to England would there be a way to just take an exam and be qualified here or would I have to take the entire course again?
-
Newbie here and new Paramedic grad. Passed boards and applying for jobs, but having a tough time. Have a BS in Bio and EMT-B but no experience as EMT-B or as a Paramedic. Applying for every job where no exp. is required; including all surrounding areas, but can't even get an interview. Any suggestions/ideas? Anyone from the Charlotte area that may have some connections? Am willing to start at the bottom, work any shift. Need to pay bills. TIA
-
I've been an NYC EMT a little over 3 years, a year and a half working transport @ Midwood Ambulance and a year and half working 911/Core @ NSLIJ. I did a small stint @ FDNY academy in between that time. I ended up resigning. I was just recently hired at Transcare's 911 division. my supervisor tried VAX'ing me but the FDNY denied me clearance to work for an unknown reason. Now I can't work 911 until the FDNY figures out why. It's been over 3 weeks. Has anyone been through this? And how much longer will it take for the FDNY to finally clear me? For what reasons would they deny someone clearance to work? And what exactly does VAXing someone mean?
- 8 replies
-
- fdny emt ems vax paramedic 911 nyc transcare
- emt
- (and 7 more)
-
Hello All, I am currently studying Paramedic Science at Northampton University in the UK and I am very curious about the following matter: It is my ambition to become a paramedic BUT it is an even larger ambition for me to move to America to become a paramedic! I would like to move to Chicago as soon as I graduate and get a job at a busy firehouse! I have also spoken to my family about this and they are going to support me the whole way! My point being that will I have to move to America and undertake the different classes that USA born paramedics have to do (IV Line, EKG's etc.)? I also have an idea to become an NHS paramedic and get some experience first? Thanks In Advance ?
-
Hey everyone! Glad I found you all, from what I've gathered from some brief browsing, this seems like a good place to get advice on the world of EMS! So, I'd thought I'd just directly ask this community some on my questions, as I'm a little on the fence about pursuing EMT and Paramedic Should I become an EMS student and eventually an EMT? Also, will my age hinder me greatly? What are the challenges of studying to be an EMT that I should be aware of? If you're concerned about the emotional and mental strain of the job, but know it is a challenge you want to try and overcome, should you think twice? Sorry for all the big questions, any answers or advice you could give me would really be appreciated! Thanks in advance!
- 7 replies
-
- 3
-

-
-
- EMT
- high school
-
(and 5 more)
Tagged with:
-
I'm going to be signing up for the NREMT paramedic exam soon and I was wondering, what are some good studyguides/websites to use to help prepare me? Thanks
-
Please leave feedback on the EMS videos we've posted. Thanks. https://www.youtube.com/watch?v=ucaCzj-nQ0M
- 3 replies
-
- Dr. El Sanadi
- Excited Delirium
-
(and 3 more)
Tagged with:
-
Hi, My name is Patrick and I'm a 20 year old EMT-Intermediate student here in Germany. After finishing my German Baccalaeurate (High School Diploma) this spring I'd like to attend Med. School. Due to the high entrance criteria over here I'll need to wait a couple of years in order to get in. Now I'm thinking about starting Paramedic training in the US this fall/next spring. I'm thinking of a 2+2 program which would entitle myself to work as a Paramedic after the first 2 years... 2nd half could be pre-med school curriculum. Before Med School I'd love to gain some hands on patient experience, routine and knowledge of a wide scope of practice! I was recommended to look for a county / state of education where EMS is not the stepchild of the Fire departments Due to the out-of-state tuition fee I'd like to attend community college for as long as possible! I was told to look at Wake Tech, NC: http://www.waketech.edu/programs-courses/credit/emergency-medical-science/ems-degree-program Could you: - Recommend me a community college in the US where EMS is taught similary? - Your favourite county where EMS is disconnected from Fire agencies? - Share your experience with international (German?) EMS students and their performance in EMS Degree Programs? This summer is fully booked from July 28th to November 3rd as I'm going to backpack around SE-Asia. Hence programs could start in the end of 2014. My current plan is to start the German "Rettungsassistent" (very narrow scope of practice comp. to a US-Paramedic) this November. Maybe your advice makes me change my plans! Give it a try
- 2 replies
-
- EMS
- international
-
(and 5 more)
Tagged with:
-
Sorry I havent posted in a while. My life has been crazxy busy.... So, I am giving a street drug lecture as a conference... as I am wont to do on occasion, and a thought occurred to me. We are seeing these "Vaping" stores, products, patients explode in numbers in this area... an exponential increase in this nich market. Even among health care providers. Now I am NOT going to speculate the pro's and con's over traditional tobacco use....But I have a question. It seems to me only a manner of time before someone puts any number of illicit adulterants in the liquid they use for this. My guess is someone, somewhere probably already has tried it. My personal bet is on opioids. But could be meth, or anything else. Has anyone actually seen this (illicit/recreational street drugs combined with Vaping) in their area?
-
Hello everyone, I'm interested in becoming a paramedic and don't really know the ropes of the field. I love to learn and would want to learn as much as possible in this field to become the best paramedic I can be.
-
My agency is seeking to improve the rescitation performance in the field, and we are generally dissasitified with the standard merit badge courses. How many of you provider either: 1- An in house alternative to ACLS or PALS/PEPP or; facilitate higher performance in resuscitation Or; 2- An in house supplement to ACLS or PALS/PEPP to facilitate higher performance in resuscitation If so, could you relate any specifics (on list or off) as far as course length and content? Also , if you are a NREMT state, what do you do about NREMT recertification. For the record, we are NOT looking at ACLS-EP. While this concept showed promise, it is logistically prohibitive to put the course on here or to train a cadre of in house instructors to the ACLS-EP level. its not from lack of trying, but rather logistical hurdles put up by the AHA. -Steve
-
In 5 short months I will be sitting in my first Paramedic class at our local Community College. One of the best programs in the area honestly, and they are developing a hell of a reputation for themselves locally. I have been an EMT for a year or so now, enabling me to have run enough CIty-ALS time to work with a medic quite a bit, run some decent calls, and learn a few things. Yet I have not been on the truck long enough to obtain bad habits. I'm one for preparation. So my question for you so far, is what can I do to prepare? My EMT-B book explains the processess of ALS Assist with tubes, monitor's and lines, and the A&P of all that, and I have been going through that lightly, but its only 1 single small chapter in the back of the book. So I'm on the quest for a A&P book. Any ideas? Any suggestions? Maybe I'm looking at this wrong? Once Medic told me I should start learning my drugs, its a BIG thing I can know before school starts its one less thing I have to learn... I'd rather refresh then learn, but I know if I Learn wrong now, that refresh is going to be a re-learn, which is twice as hard as learning it the first time. Thank You