-
Posts
2,219 -
Joined
-
Last visited
-
Days Won
41
Content Type
Profiles
Articles
Forums
Gallery
Downloads
Store
Posts posted by mobey
-
-
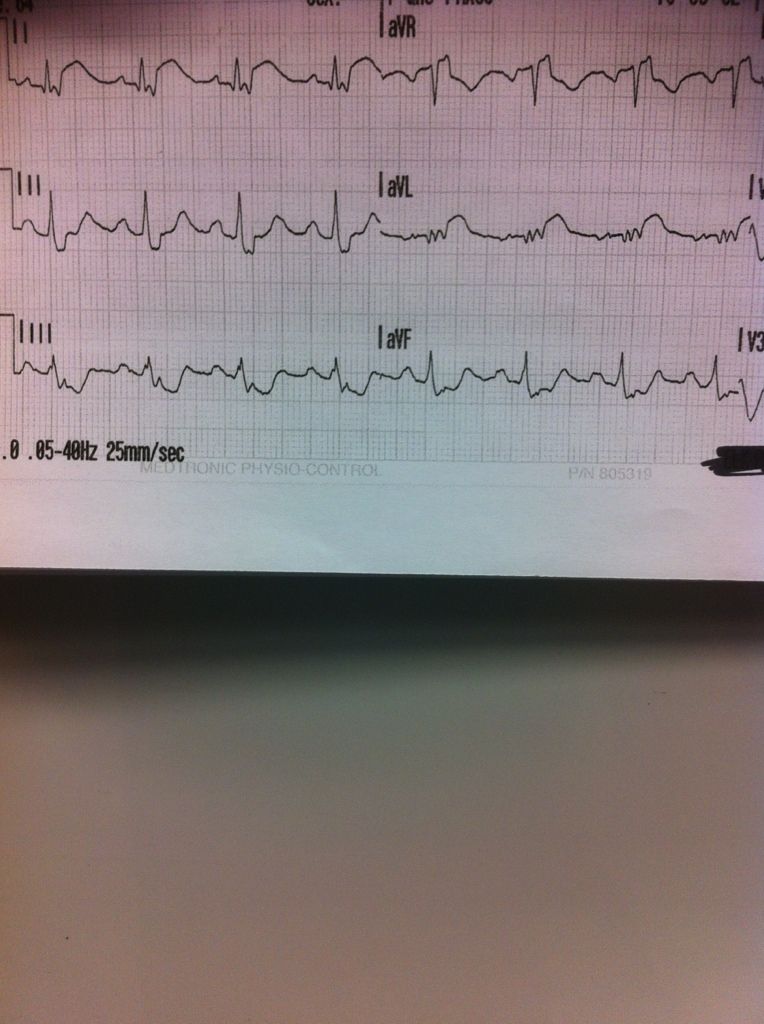
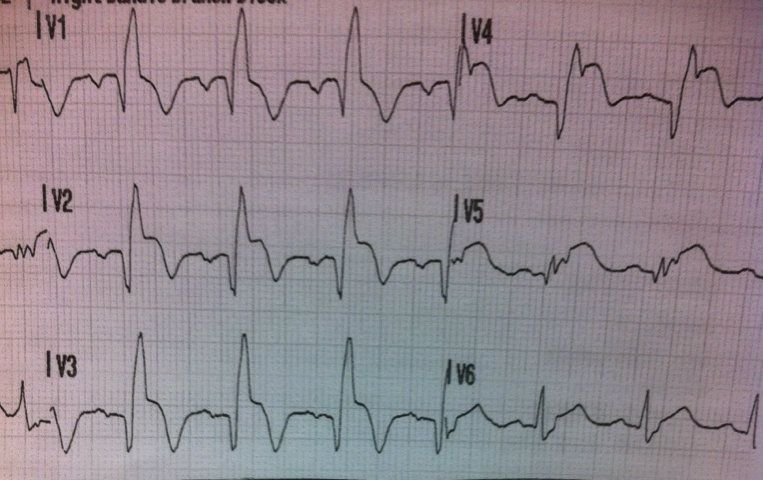
Also, the wide QRS morphology with spike 'T' waves could be caused by electrolytes which can minic an AMI, especially hyperkalemia / hypokalemiia.
Hyperkalemia can produce very odd looking EKG. Maybe, she has some renal inefficiency that has progressed?
Enough rambling.
I would:
1. Do a 12/15 lead EKG 15 not available (i didn't do one... so you don't get one hahaha)
2. Get bilateral BP's (as noted above) They are equal
3. Give her an antiemetic like Zofran IV or SL 8mg PO in.
4. Give small doses of Fentanyly for the arm pain (25mcg PRN) We have a problem huston.... You cant get a IV!
5. Give NS 500 Done
6. Watch her LOC for any changes Getting lethargic, but easily roused. More fatigue then lethargy
7. Give the N+V time to settle then give ASA PO 160mg down the hatch
8. Transport to the local ED for some more assessments and labs (mainly lytes and BUN/Cr/Tn-I).
A stop here is a good idea before a long transfer.
I would like to know:
1. How long has she been feeling unwell? Just since the seizure
2. Temp? Normal
3. Why is she on Ropinirole? I looked it up and it is for Parkinson Disease and Restless Leg Syndrome. RLS
4. Any rash? Nope
5. Stiff neck? Still back or legs? Nope
6. Splinter hemorrhages in the hands and feet? Nope
7. Decreased voiding? Nope
Cheers
Anyone want to bypass local doc-in-a box?
Also: you have the option to transmit this to cardiologist and activate a thrombolytic protocol. You carry TNK. However, the cardiologists in this program are very busy working the cath lab while on call, and don't like to be bugged unless you are pretty sure.
the temp is tympanic I assume? How is it or is it calibrated?
Once a week I drop it on the ambulance floor and kick it against the wall.... If it still works, I consider it calibrated.
-
Sorry for the delay.....
Just not tech savy
-
No trauma other than patient complains of pain in her right elbow
Seizure was typical grand maul description
No neuro symptoms
No recent falls etc.
Yes a smoker, 1/2 pack/day x25+ yrs.
General appearance is unwell. Coulor is greyish, vomiting, slight diaphoresis.

Sorry for the small pic.... not sure how to expand it.
Ctrl + should help.
-
Any advice like encouragements and reassures you guys have would be great.
OK, Then when you are ready for the non-encouraging hard to hear advice I can chime in!
-
Is she still actively seizing? if not>
How long did the seizure last? Approx 2min
Does she have any after effects from the seizure activity? Like the vomiting? Not sure what you're asking
What was she doing prior to the seizure beginning? Smoking, watching TV
Any recent illness? No
Any meds besides dilantin? Amlodipine, Metoprolol, Celebrex, Atorvastatin, Lansoprazole, Ropinirole
Whens the last time serum levels were checked? She can't remember
Any other current medical HX? Nope
Vitals? 142/90 RR20. P102 Sat 94% BGL10.4mmol Temp 36.7
BP high or normal Yes
Pupils? ERL
Blood glucose?
ETOH? No
recreational pharmaceuticals? No
Once we get these answers, then a phone call to your friend, the Doc in the box might be in order to determine if you really need to take a 2 1/2 hr ride to the city hospital with a neuro dept.
OK : I'll let someone else play now

-
Hey all, this is going to be a fairly long scenario as we follow this patient so I will break it up into 2 scenario's, I do think there are going to be many learning points for our new (and old) members.
This will be 100% accurate to what I was presented with.
You are called to a home in a remote town of 2000 people for a female post seizure. Non-priority call.
You have an acute care clinic in this town which is "closed to ambulances" due to a nursing shortage, but you know the Doc (Family medicine) that is on tonight and feel comfortable taking a patient there if you need a hand stabilizing. The Doc will not assume care of a patient though nor admit anyone.
Closest "Open" ER is 30min away. No surgical unit, no specialties. Just family practice Doc's doing thier best.
City hospital is 2.5hrs away
The home you go to is well kept, with lots of harmless animals. There is a thick smell of cigarette smoke in the air.
You are greeted at the door by a hysterical 300lb man yelling at you "My wife needs help"
You arrive to the livingroom to find a 62y/o F with her head in a bucket vomiting food.
Husband states she is an epileptic & takes dilantin. She has not had a seizure in 12 years, but just had one prior to him calling 911.
She was diagnosed epileptic 12 years ago - post hemmoragic stroke that left her with no deficits (except the epilepy).
This seizure today lasted approx 2 min.
-
oooo i see a spelling mistake in your reply on my topic its defense not defence sir
Too bad
-
i can do patient documentation with no problems passed that in my class
I won't bite this hook because I suspect you are very young.
Let me just say as a generic statement "I passed it in school" is not a good defence, either in court, practicum, or consulting experts in the subject matter.
The proof is in the pudding my friend, and I guarantee your school has not prepared you to write legal documentation regarding patient care.
-
something like that i guess and hey now im not that far into spanish yet.. im still going through grammar stuff and not forming spanish sentences yet
Of course you really aren't forming english sentences yet either

Little humor there for ya.
On a serious note, have you considered an online english writing course?
Going into EMS with terrible writing skills is going to open you up to legal problems with your patient care documentation. This will really plague you for your entire career.
-
You know something's wrong. Don't tell me you don't. Especially if it WOKE YOU UP.
Great point, and good catch in the history there!!
I dunno how I missed that. That is a significant finding.
-
Welcome William!
Let me be the first to say: Your grammar sucks!
Studying to become an EMT means more that a Bledsoe textbook. You are entering healthcare now, and it is your duty to progress your profession.
A great start is to present yourself as a professional. Eg: Neatly kept uniform, shiny boots, hide tattoos, no public obsene language, etc. When you are online you will want to choose non controversial screenames, and use proper spelling and punctuation.
Judging by your first post you have a long way to go. Luckily for you, there are many of us here that will remind you relentlessly since it is our profession too, and the way you present yourself is the way you represent our profession.
Happy studying!
-
I have not been this confused since squint & I spent a night drinking rum and talking acid/base.
What is your question?
-
Doc diagnoses anxiety issues...that doesn't feel right to me, but neither does MI...And I can't really afford to persue a long course of action if it's only for peace of mind and not based on logical, realistic concerns...know what I mean?
Nope! I don't know what you mean...
I would spare no expence on investigating a cardiac issue if you are concerned.
The reason I didn't consider it emergent, right, wrong or indifferent, is that I'm completely asymptomatic at all other times, and no n/v, chest pain, headache, dizziness, sig diaphoresis during episodes. Zero family history of hypertension/stroke/cardiac issues, plus I workout 4 times per week minimum and maintain a HR of 140-160 for 60 to 90 mins without symptoms. Shouldn't a significant pathology show itself with exertion if they are going to present at rest?
If it is exertional in nature, then yes!
If it is non-exertional in nature (accessory pathway, afib, valve issue etc) then no!
So, with those things being known, what might I be missing in the cardiac world that might cause such symptoms only three times (last time it started to ramp up, but then settled within 2-3 mins) in a couple of weeks and not at all during exertion?
To put it frankly (and a little smart-ass), Paraoxysmal Cardiac rythm disturbance of unknown etiology.
So, though it would be nice to have all of the other things done...If for no other reason so as to avoid having any fart stomping done, not going to happen on my budget. Though, I certainly will persue it more aggressively should things seem to change at all..
I highly suspect these tachycardias are going to be runs of bigeminal PVC's or PAC's, probably linked to dehydration (Poor water intake, high dose caffeine), combined with stimulants both intrinsic (anxiety, occasional adreniline shots) and extrinsic (smoking, pop, coffee, betelnut) stimulants.
But my 100% honest advice to you, is wear a frickin halter for 24hrs. I doubt the cost is too much considering these could be runs of v-tach!
Oh BTW: don't take this wrong.... but you are getting old.
Things like valve problems, athrosclerosis, aneurism, are real. Yes it would be early.... but still a consideration.
-
 1
1
-
-
Shit, first time I log on in weeks and I see this!
I will truly miss you buddy.
You have been one of the many that have made me the medic I am today, and I thank you for that.
As sad as it is to see one more of my "Cyber mentors" retire, I wish you the best, and am glad to see you leave in a positive light.
Take care of yourself
Mobey
-
Chest pain, Diaphoretic....
I'll go with 100 Fentanyl, 2.4 Midazolam and then cardiovert
If that dosent work we can try 12 of Adenosine.
If all else fails Amiodarone 150mg in 50ml minibag ran over 5min.
I do not support wasting time trying fluids of excessive vagals with that high of a heart rate, and chestpain WITH cardiac symptoms (nausea, clammy, sweaty).
Basically give them a 5ml syringe and ask them to blow the plunger out of it, if they don't slow thier rate they require further treatment.
-
With chbare on this topic, I feel nearly lnelligable to answer, but here you go:
The real question you pose is : Should CPAP be removed to administer oral medications?
First we must point out what CPAP is doing in layman's terms.
Continuous positive pressure in the incidece of COPD exacurbation is somewhat "splinting open" the airways by removing the negative pressure phase on inspiration.
The second mechansm is to re-recruit collapsed alveoli, again through positive pressure.
So, the question of removing the CPAP.
As we can see above, CPAP itself is a great temporizing measure to open up the airways, and allow better gas exchange. We must realize thoug that it is only a temporary fix. It can make a very sick patient appear well however if we do not fix the real problem (bronchospasm/secretions), then eventually the patient will decompensate...... or need CPAP for a very long time!
So you need to do a risk/benefit anaysis of your oral meds. By remoing the mask temporarily, some alveoli may re-collapse, the splinting of the airways will cease and the spasm will begin to dominate once again. That said, the speed in which this takes place will be patient dependant. However, if they die of an MI with no treatment, none of it will really matter!
This is the beauty of ALS, you post a clear cut question, and get no answer!!
I will always remove the mask to administer nitro/ASA/Plavix. For the few seconds it takes, even in full pulmonary edema, I have yet to find literature that supports continuous CPAP sans all other treatment.
Forgot to mention: Nitro drips and CPAP work nicely together fo Pulm edema!
I would do the same in this scenario. A spray or two, then start a drip.
If there was suspicion of a preload dependant blod pressure, I would (and have) forgone the spray, and just start low dose drip.
-
. It don't matter if you have boobs or not (which I do).

This post is useless without pics
-
 4
4
-
-
I'd be calling OLMC.
I personally would make a big stink, but that is my style.... I'm a stinker!
I also do whatever it takes to do what is right for the patient, therefore I would do the following.
1) Tuck in the patient, tell her to have a good night, and leave the room
2) Ask nurse for papers stating POA. * If she can't produce them, tell her goodnight & leave. If she does hen go on to the next step:
3) Get the daughter on the phone and tell her my side, being sure to use phrases like "I am not sure dragging your mom out of bed at 1am for something that may or may not have happened is best for her, and she really does not want to go" and "we don't kidnap people"
4) Get my OLMC on the phone and have him consult on speakerphone (after I speak privately with him of course)
5) By this time, the nurse should be alsmost in tears and hating her life, and that is a great time to ask "How long do you want to drag this out?" Thereby dumping all the blame for this dramafest on her and putting her in defence mode, which will hopefully result in her asking us to leave and threatening to call supervisors tomorrow.
6) Find the closest Tim Hortons, and get a large double-double in celebration of my small victory and knowing that patient is tucked in warm and cozy safe from her nurses politics.
Stinker
-
 1
1
-
-
If there is no history of alzheimers/dimentia, I would inform the patient that she may have had- exactly what that means- then explain the risks and the probability of haveing a CVA, combined with the risks from a fall
Then let her make the call. At 96 years old, who the f am I to tell her what is right for her?
Forgot too add: ECG also has to be clear, with no history of palpitations or chestpain.
-
Are any of you using Dopamine in your Non-traumatic resuscitated cardiac arrest patients, who DO have a decent BP, specifically for its perfusion effects? At 1-2mcg/kg/min Dopamine stimulates D-receptors dilating not only renal but cerebral and mesenteric vasculature. Combined with fluids to help dilute toxin buildup from a once non-perfusing patient, wouldn't dilation to these organs possibly reduce morbidity in the post arrest patient?
Not in post arrest, however in sepsis I have seen it given to "kik start" the kidneys in a non-hypotensive patient with an incresing lactate and decreasing Sp02.
-
We pick up a gentleman with this presentation a few times a year. However, I am sure this is gonna be a zebra comparatively
I am going to say get 2x IV in place TKVO for now, O2 via nasal cannula with EtC02 sidestream detector at 3lt.
Sit him up, and ask him not to cough if at all possible.
Now I'll spend a few seconds playing with the Sub-Q because it is just so cool.....
Temp?
History of a 'bleb' by chance?
Transport to closest facility with chest tube capabilities and an x-ray department. BTW: Need to know if he is on thinners, as that will change my destination.
-
Do you guys know, as we can see all 12 leads individually, if they are filtered the same as the 12 lead?
Can't believe no one has told us how to do a 9 lead yet!
The answer to this question is "No"
When you press the "12 lead" button, all filters are removed.
Since doing a 9 lead is simply moving electrodes around, but staying in "Lead II" the filter is still there, and therefore the ECG is non-diagnostic.
If you google "McL leads" you should find some decent info....
Sorry, usually I would be all over this and take the time to explain all this, but I have just taken on a new position running a station and am barely treading water this month.
-
 1
1
-
-
Dwayne i feel old...
What you are discusing is called a "9 lead" ECG. I used to do them regularly before we had 12 leads.
Back in the day Tniuqs and I had a great discussion about them on here, but it will be long gone.
As a challenge, I would love to see a new EMT-P on here describe for us exactly how to do one!
The downfall is that if you do not enter "diagnostic mode" with the machine (something that happends automatically when you hit the 12 lead button when equipped) then the print-outs are not really diagnostic because they are filtered.
This accounts for the ocasions when you see huge ST elevations when monitoring lead II, yet the 12lead shows none (or visa-versa).
Now, on to the challenge:
-
Several times they called for permission, and every time, doc said no.. Likely b/c of the difficulty to diagnose, once it doesn't hurt anymore.
I used to buy this excuse when a Doctors pain assessment was relevant to the patients surgical intervention. That ship sailed many years ago, there is no reason to have people writhing in pain so a doc can walk in and go "holy shit... his abdomen hurts, get him to CT".



Part 1 of 2 Progressive scenario
in Education and Training
Posted
Great catch!
Typing without thinking...
OK, so we transmit to the city hospital & the Cardiologist Gives the consent for SQ lovenox, but says no to the IO.
Plavix 300mg PO.
He states he suspects large MI and orders to bypass to the cath lab.
New vitals: 148/88 HR 87. Resp rate 18, Spo2 97
An hour passes, we are now about 1hr from the cath lab. The patient is quite diaphoretic and c/o new midsternal crushing chest pain 7/10. She begins to vomit again.
BP 146/70 HR98