-
Posts
412 -
Joined
-
Last visited
-
Days Won
3
Content Type
Profiles
Articles
Forums
Gallery
Downloads
Store
Posts posted by DartmouthDave
-
-
Hello,
You are an ALS crew (ACP/PCP) in a town of 70,000 people. ALS and BLS backup is available. Fire First Responders are available as well. It is winter and the weather and roads are quite bad. You have spent the morning on minor MVA's and collecting up the town drunks who are getting cold.
You are dispatched to a new subdivision on the edge of town (30 minutes from the hospital due to evil weather.....you arrive in 10 minutes) for a pregnant women in 'active labour'. On arrival you and your partner are ushered into a large bedroom. There is a hint of panic in the air.
The husband is very flustered. He states that this is his wife's third pregnancy. Everything has been going well until the last two weeks. His wife has been having a great deal of lower back and hip pain. Warm baths seem to help. When she got out of the tub her 'water' broke. The husband helped her to bed. He states that she was very weak. Once she got on the bed she had a seizure. Which has been going on for 10 minutes or more!!
The wife is laying on the bed naked. Her eyes are closed. She quite tachypnea (rate 30's). Her skin appears pink and sweaty. He arms and legs a flexed abnormally. Her toes are curling outwards. Her fingers are fanning outwards and her arms appear rigid. The patient's mouth pursed in a tight circle and her eye lips are twitching.
The patient's abdomen appears very pregnant. Their also is some staining on the bed sheets that look pinkish.
The two other children are upstairs with the patient's mother.
Cheers....
-
Hello,
Good one. I have never seen Variant Angina. Time to look it up.
Cheers
-
Pressure in right arm ~ pressure in left arm. No military experience works a desk job for a logistics company.
No radiation, does c/o "moderate dyspnea."
BGL is 150 mg/dl.
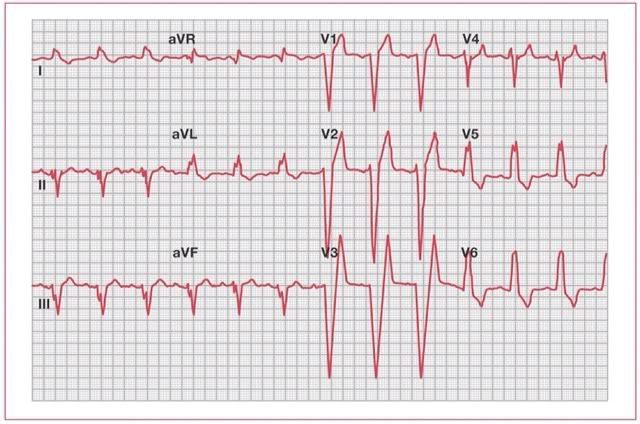
XII lead:
No xray at the clinic. You can send labs out with a local and have them back in the afternoon, about 6 hours from now. Taking an ambulance trip to the military hospital is always a safety risk.
Take care,
chbare.
Hello,
I like you thought. It could be LV strain from the patient's HTN.
According to the LIFE study that I found on Google LV strain is defined as, "...as a downsloping convex ST segment with inverted asymmetrical T-wave opposite to the QRS axis in leads V5 and/or V6."
The T-waves are opposite the QRS axis in V5 and V6. However, the concave ST is missing. Still, a solid thought.
However, can strain cause conduction delays? Could. I don't know. Maybe, coronary perfusion is limited during diastole? My CCU/CVICU experience is limited.
Cheers....
Cheers...
-
 1
1
-
-
Had to look it up. Apparently the existence of these is still controversial, but the previous theory (that conduction between the SA and AV node propagates through a homogeneous field of myocytes) does not explain the unusually rapid speed at which signals arrive at the AV node. The AHA identifies four "internodal tracts:" the sinoatrial, anterior, middle and posterior.
According to recent research (released this month- Ann Emerg Med), what 3 factors were previously regarded as risks for venous thromboembolism ("implicit" risks), but were found to have no predictive value? Extra credit: list 5 of the top 17 risks for venous thromboembolism (same article).
Hello,
Hmmmm...no access to my work account to look up the Journal. So, I will guess...
Virchow's Triad has no predictive value?
-
Hello,
Argyll Robertson Pupil (Prostitute's Pupil).....'accommodates but dose not react' =) Most common cause Syphilis...hence the name. Other causes I can not recall off hand.
Ok....
Lesion that appear on the hand due to Endocarditis?
Cheers....
-
Hello,
1. ACS (negative Tn)
2. PE (negative D-Dimmer)
3. Zebra?
-->We have treated for ACS (ASA, Plavix, NTG, O2, Metoprolol, Enoxaparin) and drawn labs.
-->We have treated reasonably well for a PE. Maybe start a Heparin infusion as opposed to Enoxaparin.
If possible, an echo/ultra sound (depending on what is available and what staff is available) and take a look at the right ventricles. I am not an expert on this but I know sometimes a PE will cause RV dysfunction. Or any other odd cardiac things gooing on.
-->No CT scanner I assume?
-->What is CMP????
I have read about the S1Q3T3(invert) rule but I have never seen it or had much luck with it.
Again, if he is pain free and stable lets not transfer this fellow until a Dx is hammer down some more. I assume the flight would be a long haul to Germany? Or, as a civilian dose a private company fly him to Saudia Arabia?? (I will have to call my brother he worked in KAF as a NO).
-->Is there a Zebra we are missing? I get tunnel vision sometime.
Cheers
-
Hello,
No cath lab I assume! =)
Also, I may be overly fatigued, but are those Q-waves in V1 to V3?
Add Plavix 300mg PO, Enoxaparin 1mg/kg, change from NTG SL to IV. Maybe top up the Lopressor (5mg was given) to a total of 15mg. Review the labs (Hgb, lytes). Top up Mg and K if need be. Consult a friend.
Any way to get hands on an old 12-lead? Was one done for a medical on a civilian contractor? Not too family contractors in A'stan. I would like to know if this is an old or new BBB.
Maybe take a look with an Echo/US as well.
Any family members have MI young?
Odd that this is the first time he 'ever felt this way.' I am not saying that a patient can not have a big MI out of the blue. But, usually, they have angina, worsening SOB, fatigue, et al......before the big STEMI. Also, his age. Possible.....but not common. If her was 56.....different story.
Wait...see if the pain come back. Repeat the Troponin in 4 hours with an other 12-lead. Be conservative. If it is a STEMI treat with TNK.
Cheers
-
Hello,
A BMI of 30. Must have been Chair Force (Air Force)....

2-3 drinks a night. Now, was that before he went overseas or while overseas?
As for sudden on set chest pain I will go with:
- PE (big guy sitting at a desk for long hours)
- Thorasic Aortic Aneurysm
- ACS
I would do the work up as posted above. Plus, check BP in both arms and if possible, is there an iSTAT (Tn-I) available in the clinic.
Cheers
-
Hello,
Herbie1,
I am talking about Vasopressin (Pitressin). As opposed to giving Epinephrine 1mg IV give Vaopressin 40 units IV during the code. Like when this poor fellow coded on CM. In theory, this may cause the varacies to constrict and diminish the bleeding. A two-for-one deal.
As opposed to a vasopressor such as Levophed, Phenylepherine and Dopamine. Stuff like that. Which you are 100% correct would be a bad idea before that tank is filled so to speak.
Correct me if I am misunderstanding what you are saying.
Chbare,
All of the SB tubes that I have seen were inserted in smaller hospitals (not sure how) and were transfer to us. One was secured to a hockey helment and two to the ET tube. Basically, the labs were corrected and the tubes were pulled and the patients scoped. I agree 100% that messing around with a SB in the pre-hospital setting or by unskilled hands in the hospital is a bad idea.
KM,
Good to know. All the SB that I have seen are just laying around. Most, looked like they were made in 1942.
Lastly.... =)
One problem that we did have with one patient was excessive pressure in the SB. There was some esophageal ischemia. Also, deflating the tube seems to pull off all the clotting that has formed as well.
Cheers...
-
Hello,
Interesting. Inderal IV. I have never seen it used for varices. I am going to look that up. Always like to pick up something new. One never knows when it will come in handy.
Could IV Metoprolol be used as well? If for example Inderal was not available?
Sorry, I wasn't too clear with my Vaso post. There is a Vaso Shock dose and a Vaso Varices dose. At the high end of the Varices dose the patient will get 30 units an hour or so.
Now, in a code secondary to a bleed push Vaso 40 units IV. In theory, it may help with ROSC and the bleed. For most ALS units (not a CCT team) this may be the only possible drug that could be helpful. Basically, what was clarified by previous posters.
I have seen three SB tubes. I have never put one in. In theory, they slide in like an OG. The one thing I have always wonder is how!! They are much more flacid than an oralgastric tube. How do you keep it from curling up. Just wondering.
Second question. Securing the SB tube. They need a little tension to keep the gastric ballon in place. The three times I have seen a SB tube the patient was tubed. Two had the SB secured to the ET tube. One, to a hockey helment. Now, how would you secure a SB tube to a patient that isn`t intubated........just wondering!
Cheers
-
Hello,
I was thinking. Vaso for shock mixed 15 units in 250 NS. With a dose between 0.01 and 0.05 units/min.
I know that Vasopressin for varacies is mix much stronger (never used it myself) and administered at a higher dose. Not sure, but I thick the dose is .1 to .5 units/min. Tenfold.
So.....when the patient coded Vasopressin could, in theory, fix two problems. That is if you had it. Just a random thought.
Weak theory. Am I off base here?
Cheers....
-
Ran on on endstage liver disease pt. with ruptured esophageal varices. As we ran the code it became obvious to me that this man's demise was precipitated by that loathsome "H" hypovolemia. He essentially bled out. The question I have for you is
"Are there prehospital techniques that can help control the bleeding of the ruptured esophageal varices?"
My simple brain says... direct pressure... then leads to How does one apply direct pressure to the esophagus? The only thing I can come up with is combitube.. maybe.
Does anyone have any tips, tricks or ideas on this one. Getting covered in Hep-C blood, doing a surgical crike and throwing everything in the box at this dude, including the the last ditch desperation Sodium Bicarb and working very very hard... never mind the decon of the rig afterwards, leads me to ask what else I could have done.
Hello,
Tough call for sure. I can not think of any tricks for this fellow. Securing the airway to prevent aspiration of blood and pushing fluids. As for a Combitube I think it wouldn't protect the airway, or tamponade the bleeding. Also, with very forceful emesis I think there could be a risk of esphogeal repture. Dose anybody have any other thoughts on the combitube?
If this fellow made it to the ED there are a few options:
1) Sengstaken-Blakemore Tube can be inserted down the esophagus and inflated. The ballon tamponades the varacies.
2) Panto IV and an infusion
3) Octreotide IV and an infusion to drop portal hypertension
4) Vasopressin (Varices Dose) infusion
5) Blood products (PRBC, FFP, ect..)
6) Endoscopy treatment and surgical interevntions
Even with all this stuff the 4-5 ESRD with bleeds that I have seen never do very well. So, really, I think you tried all that you could have.
Cheers...
-
Hello,
Good question.
I think it is safe to that this lady is dry for several reasons.
Increased work of breathing equals increased insatiable losses. The same can be said for the fever as well. Also, I am sure that this has had poor PO intake.
Physical assessment and history also shows a sinus tachycardia with marginal BP. Plus, no overt signs of failure such as edema or JVD. In addition, if I remember correctly, no previous history of CHF.
So, a 250, 500 or a 1000cc bolous of NS all would be acceptable. Depending upon protocol and transport time.
You are correct about the lungs. It would be hard to tell if you are tipping the patient towards failure. However, an improving BP and a decreasing HR in general will indicate that you are heading in the right direction.
Cheers
-
LEMON??

I have, and would again put a pt in a KED and transported semi-fowlers with suction prn. As a bls crew you do what you have to.
As an ALS provider however I think I would be more aggressive. Perhaps an awake intubation could be attempted. A large dose of Fentanyl and maybe a whiff of Versed combined with some lido spray may be all it takes to pass the cords without causing total resp depression, or at least get the laryngoscope in to get a good assessment at what your working with.
Hello,
LEMON AIRWAY ASSESSMENT TOOL:
http://emergency-medicine.jwatch.org/cgi/content/full/2005/216/1
The STARS folks came by were I work and used it with the sims. Just an assessment tool that is all.
Cheers
-
Hello,
VS? LOC? Motor/Sensory assessment?
From the description of the injury airway sounds like an issues as noted by several posters. Even more so if you put the patient supine on a back board.
Now, I am just throwing this out there;
Could you transport the patient with a cervical collar on with the head of the stretch at 30 degrees of elevation (like Tniups suggested)? Or, as an other option lay the patient in the left (or right) lateral recumbent position? Thereby allowing safe clearance of airway?
Most cervical injuries are stable enough to allow HOB at 30 degrees (with a collar) in the hospital setting. A truly unstable c-spine in general presents with deficits and even ideal care (backboard) things typically worsen as edema develops. Slightly unorthodox but easier than having possible airway issues during the flight.
The reason I am throwing this out there is a LEMON airway assessment of this fellow shows three concerning issues. First, a jaw fracture with blood equals difficult airway. Maybe there is a high grade LeFort (II or III) fracture present. Second, it would be difficult to ventilate with a BVM if the RSI failed. Third, a supraglottic airway wouldn't be helpful here as well.
This leaves a surgical airway which put you in a crap situation. Even worse, a failed surgical airway. There is an interesting case in which a CalStar crew missed a tube. Went surgical. Missed that. Then got a tube which was useless due to a large bleed hole in the patient's neck. =(
There isn't a failure to oxygenate or ventilate here (with suctioning). So, a short hop to the local small hospital and possibly deal with things there if need be. Also, with a warning the small town hospital can call in extra staff (i.e. Anesthesia). Glide scope/bronchoscope or many other options. Tube there if needed.
Also, a more detailed trauma work up is needed before the fixed wing crew arrives. CXR. AP Chest. Pelvic. And, with luck a Head CT.
Cheers...
-
Hello,
So, the decision is made to tube this fellow (good call). The plan is to use a fiberoptic scope. The patient is given a small dose of Versed (2mg) and an awake laryscope is done. It is difficult to see the cords and there is tons of dried secreations coating the back of the throat and what can be seen of the cords. The EP feels confident that he can get the tube in. Back equipment is made ready.
He is given Propofol 50mg and then Succinycholine 100mg. A #8 ET is passed without comlications. The tube is suctioned for think brown nasty junk.
The patient develops profound post-intubation hypotension (77/40) and is given a bolous and Levophed is started at 10mcg/min. The patinet is placed on the ED's ventilator. No overtly high peak or plateau pressures. A good Vm is being given.
The VS are as follows:
GCS - sedated
BP = 97/40 Map 57
HR = 144 (alram sounds.....VT...the monitor shows a wide complex tachycardia)
SpO2 = 94% on the vent
Urine = 0
CVP = 4
Cheers.....
-
Fluids to get the CVP over 8 mm Hg and hopefully that will improve the SvO2 and urine output. This is not a good time to be in renal failure.
What is the BP now? There might be a pain issue that can be addressed without interfering with the respiratory drive. The BP MAP should be maintained over 65 mm Hg.
If the ABG was drawn on a NRBM, we would use 0.85 or 0.90 as the FiO2 for the PaO2/FiO2 calculation. That gives a PF ratio of 67 which is very, very serious. Some should take not that the SpO2 was mentioned at 88% which is possible but in this situation, the SpO2 does not reflect the seriousness of this patient.
If this patient is on a humidified high flow system delivering an FiO2 of 1.0, that may be difficult to transfer. BTW, if you see a standard humidifier running of a standard flow meter (not one capable of 70+ L/M) that device will not be delivering an FiO2 of 1.0 to an adult breathing at a RR of 34. It would take at least two ("Dual") humidifiers to get a little closer to an FiO2 of 1.0. The standard humidifier with an aerosol mask, even though it may say 100% on the adjustment, will probably be delivering an FiO2 of around 0.60 for an adult with a high respiratory rate and MV.
What do those of you from other countries have available on your CCTs for high flow O2? I know Canada and Europe will generally have the better meds and technology available to them long before the U.S. Even our ICU equipment and especially the ventilators are usually at least 5 years behind your latest and greatest.
Hello Vent,
Sorry, I left out some information in my last post. This fellow is on a high flow oxygen mount that wide open. So, odds are he is getting around 60% or so. It isn't a dual system. Just a standard hospital wall mount.
His Co2 has risen so he is getting tired as you know. His VS are worsening slightly as well. GCS 14 (Drowsy) BP=130/70 MAP=90 HR=130 SpO2=82%
Urine output is still low. There was 20 out on arrival. Since then, nothing. CVP = 6 Fluid is a good idea.
Sv02 is low. His Hgb is also marginal. But some fluid should help this.
The ambulance has an LTV1000 (no graphic displays with this model...flow loops ect..)and 2 Mini Med III pumps. A CPAP mask for the LTV (I am sure they can do this...correct me if I am wrong). Plus a good selection of medications. A Zoll CTT monitor that can transduce CVP and an arterial line.
So, yes, it would be very difficult to transport this patient in a back of an ambulance on high flow. Also, I wonder if the ambulances O2 tank has enough psi in it to last for a long drive.
Cheers...
PS....Don't read too much in to the gases. I am just making up the numbers to show resp alkalosis (resp failure) moving to a tried patient (working towards a resp acidosis). =)
I should clarify, this sort of job here would be undertaken by a physician or some specalist as even our Intensive Care Paramedics are not trained to take care of somebody this crook.
The hospital would send somebody because he is on a lot of meds and things Ambulance Officers have no experience in.
Hello Kiwi,
OK, the hospital is willing to send a nurse or an RT. Your pick. The RT in this ED has intubated patients before but not for a long time (over 18 months). The RN has lots of ICU and ED experience. She worked in a larger hospital and move to a small town for a more mellow life. Also, the EP has not intubated in quite awhile as well. He can't leave because there isn't anybody to cover the ED or the admitted patients if something goes wrong.
This is why there is trepidation about tubing this fellow.
Cheers.....
Summary of Discussion:
So, give it a go with high flow O2 and hope all is well by the time you arrive at the university hospital? Or, get a tube? If so, what would be the safest way to do this? What medications? RSI?
Is this BP elevated due to a stress response from the patient? He has had a 4-5 day history of poor intake. Or, is his volume fine? Low urine output as well. Give more fluid or not? (i.e. 1000cc plus or just maintenance rate of 125cc/hr)
What extra staff do you want in the ambulance?
Any lab concerns?
Cheers....
-
Hello,
The patient wants to be a Full Code. A triple lumen subclavian is inserted and checked with a CXR. The RT inserts an arterial line and a ABG and VBG is drawn. A CVP is transduced and it is 6. The ABG shows pH 7.35 CO2 45 CO2 60 and the VBG shows an saturation of 59%.
A sputum C+S was not sent. Swabs have not been done. These are collected. Also, the patient is given Tamiflu PO as well.
BNP is not available at the lab. Small hospital with limited resources. The EP isn't keen on intubation due to the difficult airway and the frail status of the patient. Though failing the patient should be able to tolerate the transfer on high flow O2.
Cheers...
-
Hello,
I based this scenario on a fellow that was transfered to the ICU awhile back. So, as a transfer there is time to sort things out. Also, I like this scenario because the key to its success will be a collaborative approach with the hospital's staff (MD, RN, RT).
Plus, it is a situation that may rurual services may find themselves in. A complex patient in a small hospital in which the Paramedics become an important part of the hospital's team.
Here are a few ponts to ponder:
Resp status... tube or no tube? CPAP/Bi-PAP? What is the ABG telling us?
CVS..... more fluid? less fluids? Look at a sespis protocol and see how it can fix this patient.
Labs..... low K and Mg 40mEq KCL in 100 cc was given once... Needs more or less K or Mg? Any other labs to check?
Social.... He is very sick. Prior to transport what should be addressed?
Support.... The hospital isn't keen on sending staff. Maybe an RT or a RN...maybe =)
Lastly, your ambulance is stocked with a wide range of drugs and equipment (i.e. IV pumps, CPAP, Transport ventilator).
I am missing something... What is the point of this post? Is there a question or game we are supposed to participate in?
I see a case presentation with diagnosis and treatment already in place. What are we supposed to do?
This is true. He has been in the ED for 2 hours. It is an hour or so to the receiving hospital. Is there more than needs to be done? Is he ready to go? Other Dx to be considered. This may not be a 911 scene call however there are few things prior to leaving that may maximize ones odds of success.
I just wanted to give something a little different a go!
Cheers...
-
Hello,
Location:
You are an ALS crew in a small town (population 5000). It is 1000hrs and you are dispatched for an urgent transfer to the local University Hospital. The University Hospital is 125km away.
On Arrival:
You are greeted by the ED staff and are given a report. Mr. Smith is a 67 year-old male with an extensive and complex medical history. He has had a MI in 1993 (NSTEMI),CABG in 1994 (4 vessels), PSVT, HTN, DM I, Dyslipidemia, Depression, Renal Insufficiency, Esophageal cancer that was managed surgically in 2008 with a Esophagectomy as well as Oropharyngeal Squamous Cell Carcinmona (OSCC)in 2009 that was managed with radiation and surgical interventions.
Since 2008 the patient has had dysphagia and numerous aspiration pneumonia. He was made NPO. A PEG was insert in Dec 2009 and the patient was started on bolus feeds. However, he has still had trouble with aspirations. There were plans to advance the PEG in to the small bowel.
For the past five days the patient has been feeling unwell. Chills, myalgia, fever, and a hacking cough with some think yellow sputum. His wife was concerned that he had a pneumonia. The patient has been refusing his tube feeds because he feels unwell.
The patient did not want to go to the hospital and took some old antibiotics he had around the house. This morning he tried to eat. His wife started his tube feed at 0800hrs. Shortly after feeding began he started coughing and threw up. Gagged for awhile and trued 'blue'.
He developed respiratory distress and was driven to the hospital by his wife.
On Exam:
The patient is sitting up in bed (75 degrees) and looks distressed but is lucid. Numerous old surgical scare are seen on the patients neck and jaw. He seems to have a poor range of motion as well.
GCS 15
PEARL 4mm
Strong x 4
BP 180é90
HR 120
Temp 38
EKG: Sinus Tachycardia with an old RBBB
RR 34
SpO2 88% on 100% FiO2(humidified oxygen wide open)
Lungs - course crackles
Abd is soft
Foley is in situ with 20cc of concentrated urine
There are 2 IV. An 20 gauge in the left hand and a 18 gauge in the left arm
CXR shows a white out on the right side and cloudy looking left side.
Labs are limited. They show:
WBC 24
Hgb 84
Na 137
K 2.9
Mg .85
ABG show (100% oxygen):
Ph 7.45
CO 32
O2 64
BE 2.2
He has been Dx with Sepsis and aspiration pneumonia on a preexisting community acquired pneumonia.
Treatment thus far:
1L NS bolus
40mEq KCL IV
NS+20 KCL at 125cc
Vancomycin 1gm
Pip Taz 4.5 mg
Zythromax 500mg
Decompressed his gut via the PEG
Zantac 150mg IV
His medications are:
ASA 80mg od
Lopressor 50mg bid
Lipitor 40mg od
Ramipril 5mg od
Sliding Scales Insulin tid
Tyl prn
Advil prn
Lansoprazole po od
Motilium 10mg po tid
Cheers...
-
 3
3
-
-
Hello,
Sorry for the above post. I was AFK and when I came back it wouldn't let me edit. =(
I never considered the issue of quality control or errors. From my experience I haven't seen any EMS services draw labs in the field. Or, use iSTAT technology.
Cheers...
-
In the U.S. that may be harder to regain the confidence of the agencies that govern quality control for labs. Too many foul ups with poorly trained individuals with improper specimen collection and handling techniques led to incorrect and sometimes fatal treatments from the lab results. Even labeling was an issue with some EMS providers failing to see that their specimen was correctly labeled in a timely manner to get the correct labs results on the right patient. The EMS agencies themselves could not provide evidence of any training or QA monitoring for this "skill". If they also fail to monitor intubation skills, lab draws probably won't be much of a priority either. Even for Specialty, Flight or CCT, we may have the lab at the sending hospital draw the specimens and fax or call the results to the MD at the base facility which can then be relayed to us during transit. If we have extra cartridges for the iSTAT to do different labs, then yes we may draw and run the specimens immediately for certain tests. However, if the transport is more than 30 minutes, we have to take into consideration the length of time, proper storage and exposure of certain specimens if we must transport them.
At one time EMS prehospital lab draws were not an issue but as with anything, when you let the lowest common denominator represent the rest of the flock, eagles can quickly be viewed as turkeys when it comes to soaring to new heights. Even the hospitals and clinics have raised their standard to where the phlebotomist that had once been OJT must now have at least 140 hours of education/training in just phlebotomy and they now have a national certification gaining popularity that reflects the national lab standards. That's longer than the EMT-B in the U.S. Any licensed hospital employee (RN, RRT) must now show initial and yearly competency in lab specimen collection. There are also agencies that do check and ensure this process is carried out. EMS still has not achieved that level of oversight in many areas and there probably would be some union that would say any additional education or competency expectation is unfair and someone is picking on them or treating them like criminals (to quote the LA FF article).
-
Hello,
This case is based on a fellow that came through the hospital. I altered it to fit better as a case study. I picked a suburban/urban setting because I wanted to work with an environment that most poster would be familiar with. A major hospital 10-15 min away. Something like that.
Now, with longer transport times (ground or air) starting abx would be essential. Early abx improves outcome. I agree with this 100%. Now, how to make this happen...that is an other story.
Prehospital labs: I like this. It is a good idea. Makes for a smooth transition from EMS care to hospital care. Heck, if you are putting in a line pull a few tubes off as well. Toss in a few blood cultures as well, if needed Inexpensive. The skills are there.
Cheers....
-
Hello,
So, this guy went to the OR and everything was excised (penius,rectum, and surrounding tissues). A VAC dressing was inserted as well as a suprapubic cath. Plus, a colostomy as well.
He had a high APACE II score and did poorly. He was tx with lots of IV fluids, abx, Levophed, Dopamine for a low SvO2, and APC. He had a slow, painful and problematic recovery. Developed ARDS. Was placed on ARDSNET. The works....
A pile-o-problems. Took months to get out of the ICU to the Sx Ward. I wonder what happened after that.
I like this case for a few reasons. One, it was a BLS crew that responded and they actually 'exposed' and looked and knew things were going bad. Because they did a good physical assessment. Second, it shows how EMS can compliment ED care if done right. On arrival, the 1st 1000cc was in and the ball was rolling in the correct direction.
Cheers...



The Baby and the Blizzard
in Education and Training
Posted
Hello,
The husband is moved out if the room and the anxiety level drops greatly.
You do an assessment of the patient. She is able to open her eyes and looks at your. She has some trouble talking because her mouth is 'cramping'. She says her arms and legs feel 'numb' and 'cramped up'.
VS are:
BP: 150/90
HR: 110 NSR
Resp: 34 Rapid and deep
SpO2: 99%
Temp: 37.5
A head-to-toe assessment findings:
General Impression: A fit looking 29 year-old women who is obviously pregnant. An old hospital ID band in noted on her right arm.
CNS: Her arms are still rigid and her fingers and toes are fanning outwards. Her mouth if fixed in an 'O' shape. She is lucid but says she can not get her arms and legs to, 'Do what she wants them to.' Her pupils are 5mm and reactive. She is quite anxious and is complaining of numbness in her arms and legs.
Resp: Lungs clear as a bell. She is taking large deep breaths.
CVS: Skin pink/warm/dry EKG shows Sinus Tachycradia
ABD: Quite pregnant
History:
The husband is able to offer some history. This is her third pregnancy. The first two went to term and were delivered vaginally without complications.
He thinks that his wife is at 38 weeks right now. For the last two weeks she has been seen at the hospital three times. The last time two days ago.
Her chief complaint during these visits were lower back pain and left flank pain. No problems were found and the pain was due to the baby's position. She was given a script for Tyl#3 and Oxazepam 15MG QHS for trouble sleeping.
Her last GP visit was last week. The husband isn't sure what was said. But, his wife said everything seemed fine.
She has no medical history.
Cheers....