
medic001918
-
Posts
417 -
Joined
-
Last visited
Content Type
Profiles
Articles
Forums
Gallery
Downloads
Store
Posts posted by medic001918
-
-
Please explain your interpretation of this strip.
What else are you looking for? A number of experienced posters have commented on the strip and how those answers were arrived at, and more importantly why the answers aren't definitive. Let us know what you're looking for, and we'll try to help. It seems as though quite a few people have offered an interpretation of thise EKG and explained what they've seen (with axis deviation, etc).
AZCEP, I was going to mention procainimide but I know it's been recently removed from the ACLS guidelines and effective July 1,2007 they're taking it out of our protocol entirely. But if you have it, it's certainly a viable choice along with the beta blockers.
Was the patient tachycardic like this upon your arrival? Or did it set in after you got there? If the patient had that kind of a rate when you showed up, a 12-lead should have taken precedence over other intervention to ensure that the shortness of breath isn't due to a cardiac problem. The shortness of breath of a cardiac problem needs distinctly different treatment than someone with that of a respiratory etiology as I'm sure we can all agree on.
Shane
NREMT-P
-
Stupid question, but are there P waves? it kind of looks like there are but it's hard to tell. Also if it is, could it possibly be 2:1 AFib with an aberrancy?
You mean an a-flutter with 2:1 conduction? Not trying to split hairs, but the "fib" in a-fib is not a distinguishable p-wave to count as a conduction, whereas a-flutter has the distinct flutter wave that can be counted. Without having the strip physically in front of me, it looks like it's fairly regular to me, which would decrease my suspicion of a-fib (but not a-flutter since a-flutters with consistent conduction such as a 2:1 or 3:1 may retain regularity).
It's hard to tell from the poor image, but it looks like it could be an SVT with a bundle branch block? You said you didn't get the chance to do a 12-lead because this took you by surprise, but I'd like to see what the strip looks like from before the tachycardia set it. Does it look to be a narrow or wide QRS when the rate is controlled? If it's wide, then there is a strong possibility of a bundle branch block and I'd lean more towards the SVT. If it's narrow and then developed a wide complex tach, I'd go more with V-Tach. It's difficult to tell without seeing a 12-lead on this patient.
One thing I'm curious about, how much distress was the patient in while you were treating for pulmonary edema? I know it's in our protocols (and generally good practice) to obtain a 12-lead on patients complaing of shortness of breath. If the patient was in severe distress, it changes the priorities a little. But if this was a patient in mild/moderate distress, a 12-lead would be expcted of us.
So how did you treat this patient and why? I'm thinking there's a medication that is carried by many services that works on atrial and ventricular rythems...Amiodarone wouldn't be a bad choice for this patient depending on the rest of the story. It's hard (if not close to impossible) to base a treatment off of an EKG alone.
Shane
NREMT-P
-
Any of these services will give you the opportunity to obtain the emergency experience you desire. The transfer's aren't that bad...they are part of the job in the area for most. Especially as a new medic. As you gain experience, it will open the doors for you to go to other servies.
The service's in Hartford are American Medical Response (North End) and Aetna Ambulance (South End). AMR offer's the opportunity to transfer to other ares in the country should you choose to do so.
As far as licensing goes, I'm not familiar with the process coming from Mass. A call to CT OEMS could answer that. I believe with the National Registry card, you might be all set. At the most you'd probably have to take the written again. I don't know for sure so don't hold me to it.
Other services in the area that aren't fire based but offer good experience are Middlesex Hospital and Windham Hospital. Both generally require 3-5 years of experience though to get on the job. You can also check out New Britain EMS. They are a great service to work for (I also work part time for them) that does a lot of teaching and has even more progressive protocols. It can be one of the more difficult services to obtain employment with in the area though. Their website is www.nbems.org if you want to check them out.
Good luck,
Shane
NREMT-P
-
I'm a paramedic in the Hartford, CT and actually worked the city for three and a half years. I'm still technically employed by the EMS provider there, but am contracted to one of the suburbs. I still have knowledge of the area and the system. Hartford itself has EMS provided by two commercial services. The pay is on par for the area with a new medic making in the neighborhood of $18-19 per hour. It goes up from there based on experience. There are some fire departments in the area that provide fire/paramedic services, but those tend to be few. Much of Connecticut BLS transport is provided by volunteers, and commercial fills in. There are a few private services that hold the PSA for certain areas as well. But they tend to pay less than the commercial services.
As far as recipricosity, Connecticut is a national registry state. How it would reciprocate for you would depend greatly on where you're relocating from. Without that information, it's difficult to answer the question.
Call volume in Hartford is up on the average. It does have a reputation as a violent city statistically. You will build experience quickly, but be prepared to do the transfers that comes with the services that cover the area. To work in the city as a paramedic, there's no way around it.
Without knowing your experience level, it's difficult to gauge the learning curve involed with the move. There's too many variables to your questions to get accurate answers without knowing more about you.
All in all, it's not a bad place to get good experience quickly. You'll learn a lot. In Hartford, there's not other paramedic service (such as the FD) that will back you up on calls. Some commercial services provide transport for the fire departments that also provide their own ALS and this limits the exposure for a new medic since the FD has precedence and can tech the call which will make you their EMT essentially or leave you driving. There are some good providers, and there are some bad providers. The protocols tend to be rather progressive allowing for quite a few treatment options. They aren't totally "cook book" protocols full of "it/than" statements. They are open to interpretation.
Shane
NREMT-P
-
Not commenting on the case presented here. I dont really know the situation.
When did it become a medical emergency to be intoxicated, or un-lawful. If you are over 21 not a threat to yourself or others, not incapacitated enough as to not being able to protect your own friggin airway, or sitting in the middle of the road pissing yourself and reciting the lines from a christmas story.
I like to party a little, do I need an intervention? Mental health evaluation? A bed in an ER thats already strained, understaffed and full of people that for the most part require hospitalization.
If your not underage, not a threat to yourself or others. You dont require a bed in the ER or a cell at the police station.
Then again medicine is now driven by liability. If there is a chance you might be held responsible. You have to err on the side of caution. Its bullshit.
So I have to get up every twenty minutes to haul a drunk to the ER because everybody is worried about getting sued. Even though the guy has no business being in an ER. There not babysitters, and I am not the party train.
I'm inclined to agree with Whit on this matter. The presence of alcohol use alone doesn't mean that someone is not capable of understanding the consequences of their refusal. There's a difference between someone who's incapcitated due to alcohol use and someone who is just having a good time. Ultimately, it comes down to judgement and documentation of how the call went down. A patient could certainly make a good case if he was able to understand his actions and decisions, and was forced to go to the hospital anyway.
If someone has threatened harm to themselves or someone else, that's a different matter entirely and then the hold of the patient becomes more on a psychological issue rather than the issue of intoxication. This is the kind of case where they could transport. She took an overdose of medication in an attempt to harm herself. That changes it more to a suicidal or psych issue and they are absolutely correct in transporting her. To not intervene with this patient would be negligent.
Shane
NREMT-P
-
So sometimes people had to wait 20 minutes for an ambulance. If residents would learn about these issues BEFORE moving into an area some of these issues wouldn't occur in my opinion.
Well I agree that people moving to an area should research the available resources, there is also a responsibility of a service that's already in place to provide reliable, time effecient responses. And I'd be willing to bet that somewhere on paper there's an agreed upon response time between the service and the town. It's a question of how much that repsonse time requirement is enforced. To blame the person for living in an area that provides unprofessional and poor services under the banner of being a licensed emergency service is very much out of line. Maybe the town should recognize the problem and step up and address the matter. That might be a better thing to have happen than to have the potential resident have to figure it all out on their own prior to moving there.
Shane
NREMT-P
-
Why are you striving so much for a glorius (if not bloody) image for EMS? That's not what we are, or even what the job is like most of the time. While I think your intentions are good, I think your means of trying to affect change is wrong. While it might not sound as intense, public information and education is a much better means of making the public aware of what we do and how we operate. Ever offer to go to the senior center, school or any other public assembly in your service area to offer some education and general information? Do a blood pressure screening clinic for the community. Talk to people to raise their awareness. This idea of trying to improve our image with the dramatic, bloody, life saving call is only going to lead to the public believing we are something that we are not in reality. Do those calls happen? Absolutely. Are they common? Not a chance. Let's make improvements of our public perception by being honest with the public about what we do and what our role is in their healthcare; not mislead them to make us seem more glorious then we are. A well presented public display (seminar, open house, etc) will form a lasting opinion and impression on those in the community that you serve. Like I said before, pursue that as a means of causing a change rather than the misleading glory photos that you so desperately seem to want in the news.
I'm okay with quietly remaining in the background and knowing how I fit into the healthcare system if the only alternative is misleading images of what the job is like and what we do.
Shane
NREMT-P
-
No one knows anything about EMS except we must all be scum. Seems the only publicity we get is the bad. For example:
#1 How the hell could someone like this be allowed in EMS or even as a lowly FF. With convictions should be out in the cold. Sorry have no sympathy for child molesters. This is all the publicity we get, the bad, the mistakes.
First of all, if you're so concerned about our image let's not resort to bashing "lowly" firefighters. Let's conduct ourselves as professionals and extend to them the professional courtesy that we all seem to desire oursevles. While the majority of us might agree that firefighter's don't make the best EMS providers, they do still provide a valuable emergency service in the arena for which they are trained.
#2 We really need to find ways legally around the big old HIPPO so we can let people see what we do. Telling them does nothing. Why can't we get film out like LE and FF that makes it look like we save lives on every call. People want to see action, drama, blood, and guts or they assume we do nothing. Why do people back FF and LE, it is because they publicly display the most dramatic scenes. They do not just tell people we go put out fires etc, Or we occasionally shoot bad guys, no they get footage out there. In EMS basically all we can do is give stats to the public. You tell me you did cpr means nothing, but if had video in background of us shocking, pumping chest, intubating, lots of drugs and other equipment visible, it becomes real. If it's being done on dummy not going to cut it. For us to be seen as a must have service like, LE and FF, we must find way for the public to see us in action. The public doesn't seem to understand that LE and FF rarely do the things that make the news thats why they have no problem giving money and support. EMS is never seen so we must be doing nothing to benefit, we're just taxi drivers, so why give us money or support. The videos we need out there are usually the futile ones, the ones we will never get back but do the most work so requesting signature authorizing us to use video and photos ain't going to happen. Just today on the news so FF that in my opinion made some bad choices but got some great publicity because they came diving out of burning building. I can almost bet that will be used in some publicity add soon, more money for FF's. Look at the popular movies, the pay per view events, what usually does best is the action packed blood and gore.Like Rid mentioned, do you really want camera crews following you around all the time filming your day to day activities hoping to catch a few minutes of sensational film? As far as hollywood movies, the action is what people want. And even in a significant medical call, the action just is not that captivating to keep the attention of an audience. Look at most of the ER type shows on TV (the shower ER and such), they focus more on personal conflicts and relationships then they do the medicine. Why is that? It's because the medicine goes above the head of most people and it really isn't that exciting. A police officer arresting a bad guy; most people know enough about the law to know when someone is the "bad" guy. A firefighter putting out a fire; people know what fire is and they know it to be dangerous. A paramedic treating an MI or a patient in CHF; not so exciting unless you intimately know the job.
Just like FF and LE most of our day to day activities suck but we need to be able to show the good ones so people will recognize we exist. When people think of EMS almost all assume that we are FF, yuk, spit. I once was a firemonkey and respect the work done and don't blame them for taking advantage of all the good video to milk the public for all it's worth.Another point as far as day to day views and thoughts of EMS compared to the FD and PD is that people think of them more often because as a society we tend to be more concerned with our physical possessions then our health. The FD and PD are the services most people think of when it comes to protecting these valuables. EMS is like an insurance policy, you don't know how good it is or how important it is to have one until you really need to use it. And after that, it's too late to start thinking about what should have been in place.
We need to find some way to get our rare good calls out in public to.Why?
Sorry about the rant.EMS lawyers on here provide some guidance how we could legally do this. Help us find a way to actually let the public see what we do. People need to see us working on real patients, they don't want to read stats.
If you really want to do this, why do you need to have an lawyer offer guidance? Get together with your service and work to improve the image and more importantly to provide public education about what we do. Hold open houses at the station. Be active in the community. Go to a local sports game and just open up your truck for people to look through and ask questions. Make sure you're dressed appropriately. Be professional and polite. Work with other agencies in your service area and start a program like www.everyfifteenminutes.com. This would allow the public to see a "dramatic" call, show that we work along side the PD and FD, see what we're capable of, help to increase the effects of driving while intoxicated and bring your service to the front line of the community that you work in. In fact, I'd be surprised if the local papers didn't run a story if you started something like that.
The guidance and knowledge of how to change our image is there, it's just that the majority of people don't want to put in that much effort since this is a stepping stone to something else for most people and not their career.
Shane
NREMT-P
-
The nurse is taken away in handcuffs by the police officer.

You elect to synchronize cardiovert anywhere between 50 to 100 j (your preference). A 12 Lead immediately after the cardioversion shows:
During transport you do another 12 lead, this is what you see:
Vitals: P: 100 and regular, R:20 and a little more relaxed, BP: 108/70.
Soon after you take the second 12 lead she complains of palpitations and you look over at the monitor and see this identical rhythm:
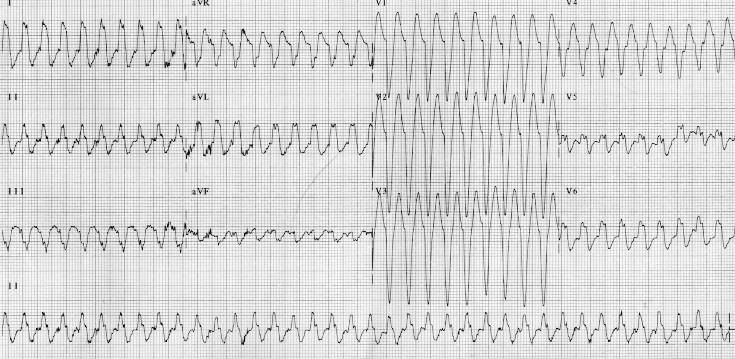
Vitals remain unchanged, RR increases slightly. No other complaints/changes. You are 5 min away from the ED. What next?
Would you have done anything differently looking back?
If we're going to call this V-tach or even if we're still not sure of weather it's an SVT or V-tach it would have been appropriate to push a loading dose and initiate a drip for this patient of an antidisrythmic medication. Since it doesn't appear that we can conclude V-tach vs. SVT, amiodarone would be a good choice as it works on both atrial and ventricular pacemakers. After conversion, a loading dose of 150mg IVP over 10 minutes would be more than appropriate. If you're set that it's V-tach, then lidocaine would be appropriate. The second 12-lead posted looks to definatly be V-tach to me. So in that case either would work. A loading dose of 1 to 1.5 mg/kg IV followed by the appropriate maintainence infusion at 2-4 mg/min would work well.
Shane
NREMT-P
-
No need to apologize for calling me a smart a**. I didn't take offense to it. I'm not familiar with the canadian system and their levels of training. So I wouldn't know what someone trained to your level is capable of identifying and what they're not with regard to cardiology. It was quite possible that the blocks are beyond the training and education that you had been given.
But in order to prevent this thread from falling apart over semantics, please accept my apology.
Shane
NREMT-P
-
Careful Shane, your making some pretty brash assumptions and are being quite offensive. Maybe inquiry would be prudent before making assumptions?
We are a larger (~20,000 calls/yr) urban ALS system, most of our basic EMT's are also trained (and reasonably proficient) in ECG interpretation, our medics teach ACLS to the doctors. Our organization is quite up to date and progressive when it comes to cardiology, so don't be a smart a**, we know what a block looks like!
It wasn't an assumption at all. In fact, if you read closely you would have noticed that the entire thing was phrased as two questions. And you'll also notice that I was not bashing either, I was just looking for the rationale. The initial post was rather vague in an attempt to aquire information. And based on what was posted it sounded very much like the basic heart blocks that have already been presented as possibilities. Make sure you look at the entire post before getting worked up and taking offense. They were questions...implying that I was looking for answers. If it were an attempt to bash you, they would have been statements.
For an example, you can look here: http://www.madsci.com/manu/ekg_hypr.htm under left atrial enlargement.
But since you've provided some more information to work with...let's see what we can come up with. Is it possibly a biphasic p-wave which would be indicative of atrial enlargement? There are biphasic p-waves that appear to be two p-waves side by side without breaking the isoelectric line.
Shane
NREMT-P
-
You wanted advice; here it is: spell correctly, capitalize, use apostrophes, know the difference between “alot” (misspelling of “allot,” which means “to distribute”) and “a lot,” know that “your” is possessive while “you’re” is a contraction of “you are,” know that “any way” refers to one of multiple ways and “anyway” is a synonym for “anyhow,” realize that one of the reasons your (our) generation is thought of as lazy is because your (our) writing is lazy, punctuate your sentences in a not only technical, but also stylistic manner. Good written communication (different than well written communication) will get you further (an abstract distance, opposed to the physical distance described by “farther”) in a career as a federal agent than an EMT license will. Good luck.
Nice first post. I like it.
Shane
NREMT-P
-
I agree that it's hard to speculate with what little information has been posted. My initial thoughts are an a-flutter with 2:1 conduction or a second degree type II (mobitz) block. Or quite possibly, maybe even a third degree heart block?
I'm curious without knowing too much about your system, but why are you doing cardiac monitoring if you don't know some of the basic rythems that can be determined by a three lead EKG? The flutters and heart blocks are common entry level cardiac rythems to determine and have been taught in every cardiology class I've ever taken? I'm not bashing here, just looking for the rationale.
Shane
NREMT-P
-
why not? isnt there some sort of law that says you are supposed to help out, correct me if im wrong. i know there is a law saying you cant be held accountable for helping.
There is no law in most states (not all) that says that you are supposed to help out. I believe Vermont is one of the states with a law that says you have to stop, but that's not just limited to trained personnel.
The law about saying you can't be held accountable for helping disappears as soon as you identify yourself as a trained rescuer. That means you received formal training in emergency response and will be held to that standard. The good samartian law covers civilians.
Shane
NREMT-P
-
However, the most important thing I carry is a cell phone so that I can activate the 911 system.
Well stated. Isn't part of the EMT course knowing when to request more resources? Last I knew, it was included. So by yourself, with only a little bit of gear (and not one of the most important ones; such as the ambulance itself to transport), you need additional resources to correctly handle the situation. The cell phone is one of the best tools to have for that.
Otherwise, I agree with others about education being more important than supplies. If you really want to help as a first responder, know how to perform an accurate and thorough assessment so you can have a decent report for the crew that does show up to handle the call. If you have all the toys, and no decent assessment skills or report ready then that would make you nothing more than the joke of that call. Take some anatomy and physiology if you want to spend your money well.
Shane
NREMT-P
-
I'm just simply stating what my instructor drilled into our heads over and over again. He is and has been a medic for 30 yrs in this state. He said without a proper DNR we have got to start CPR. It may be that we are told to stop but we must, without question, start CPR if the family cannot provide a proper DNR.
Josie
That's not what you said though. Without a valid DNR, you must begin efforts. But what you said was this:
We were also taught that even if med control tells us to discontinue CPR our scope of practice tells us we are NOT allowed, only ALS can make that decision.The common interpretation of that statement is that even if you call medical control, and they tell you NOT to work the code...you're going to work it anyway and violate a physicians order which would be higher than that of a paramedic.
Shane
NREMT-P
-
It was so cool to find this, my instructor gave us almost the exact same scenario. According to the protocol here if there is not a valid DNR we are to start CPR and call for ALS. We were also taught that even if med control tells us to discontinue CPR our scope of practice tells us we are NOT allowed, only ALS can make that decision. (It's our butt that can fry regardless of what the doc tells us) So legally we have to do CPR even if morally we want to just let him go in peace.
So you have to disregard an order from a doctor to withhold resuccitation and wait for a paramedic to make the determiniation? It seems to me that medical control would be a higher authority then an ALS provider in the first place. In a case like this, it's not like medical control is giving an incorrect order that's "harmful" to the patient that you would need to disregard. That just sounds like a totally strange protocol. I don't know as though I'd want to deal with disregarding a physician's order and wait for one from a paramedic. It just sounds like a strange system to me.
Shane
NREMT-P
-
By that, I am asking what sorts of jobs are available to medics besides the trucks and working in the er way below their training? I ask this because I start school 5/29 and I am just curious what folks do if/when the EMS life wears them out.
Thanks.
Isn't this the kind of question that should have been answered prior to entering (or agreeing to enter) paramedic school? It just seems to me that before you invest the time and effort into becoming a paramedic, you would know what your options are.
All of that being said, as others mentioned there are industrial jobs, ER jobs, etc. Another avenue would be to pursue becoming an educator for EMS. Or completing the educational process for some other line of work so that when the time comes, you're prepared.
Shane
NREMT-P
-
Ok. I gotta ask. How does hydrocodone affect Carbon Monoxide (CO) levels in a patient?
I can't find anything that supports this idea. Can some help enlighten me? Or was there just some mistyping going on above?
-be safe
I was wondering the same thing myself.
Shane
NREMT-P
-
Do we need to visit this again???
Apparently we do, since some people just don't seem to get it.
Shane
NREMT-P
-
We use Etomidate for intubation at a service I work for and it has worked well when used appropriately. As far as for patients with a suspected head injury, it's in our protocol to give 1-1.5 mg/kg of Lido IVP prior to Etomidate and the intubation attempt.
One of our contraindications for the use of Etomidate is the presence of trismus though, since it's not always going to relax it enough to facilitate the tube (if it ends up relaxing it at all).
We've only had it in the trucks since 02.01.2007 so it's pretty new to us but it's been used a few times with good results.
Good luck,
Shane
NREMT-P
-
While the desire to keep yourself and fellow crew members safe is admirable, it's difficult at best to "show" you how to protect yourself from these patients on an internet forum. The best asset you have on any call is your senses and those little "feelings" that you get. Keep a keen eye and know when things just don't seem right. In time, the senses develop even more so.
As far as when things get physical, your best bet would be to pursue some sort of self defense classes locally that would be of benefit. You may be able to get a deal through a local business if you approach them. I can't really describe how to perform some of the techniques, but I can do them physically after 5 years of martial arts when I was younger.
Shane
NREMT-P
-
Given that the narcan was going to have a temporary effect, and the redosing was going to be difficult considering the movement described, wouldn't it be prudent to secure the airway and move the patient to the transporting unit, leaving the titration of the narcan to the ER in a more controlled setting?
Once the airway is secured, I'd have a hard time pushing any narcotic antagonist that I knew would wear off before the opiates did.
Without details in regard to the extrication from the house, the narcan shouldn't wear off prior to that being able to be accomplished in the majority of cases. If it's a complicated and prolonged extrication that would change the scenario a little bit. I'm still thinking that for most extrications, it shouldn't become an issue.
Shane
NREMT-P
-
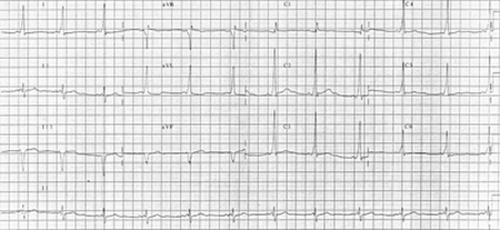
There's really no story on this one, I think I got it from class. Just going through the butterfly collection and thought I'd share.
I didn't black out the machine interpretation because, as most of you probably know - and if you're new you should find out - those interpretations are not always accurate. Usually I disregard them all together. I have a great strip that illustrates this... just how wacky the interps can be... i'll try and post it.
This is indeed sinus tach with a LBBB. The ST elevation is characteristic of a LBBB. There are however a couple of premature beats (beats 3 and and 3rd from the right). I think they are either PVCs or PACs, I think those are P waves... i dunno.
Based solely on this 12-lead I was looking for treatments for ischemia... Even if my patient was asymptomatic, i'm still going to give 324mg ASA and maybe some nitro (pressure depending) and you bet you socks O2. This is a very concerning ECG, a ischemic heart beating fast, throwing premature beats. I would also wager on an underlying MI.
Thanks for the comments!
Based soley on this 12-lead, I wouldn't go treating for ischemia. This could be, and most likely is a normal variant for this patient. Without a cheif complaint to go along with the story, it just doesn't look like an MI to my eyes. Giving some O2, sure. Giving some aspirin, maybe. Giving nitro...no way. This is one of those things that you need to look beyond the monitor and look at the entire picture in determining your treatment. If you're going to treat based soley on a 12-lead, you will at some point cause a significant complication for a patient needlessly. Hopefully this was just an excercise and not something that you would never do to an asymptomatic patient in the field.
And I'd wager against you and your MI diagnosis. I'm going with normal variant.
Shane
NREMT-P

A&E Intervention: Medics can accept refusal from a drunk
in General EMS Discussion
Posted
So anyone that's had a couple of drinks can't refuse your services? It's not really as clear cut as you try to make it seem. The presence of alcohol doesn't render someone in capable of making informed decisions. There's a difference between being incapacitated or unstable due to alcohol, and someone that's had a few drinks.
Shane
NREMT-P