-
Posts
452 -
Joined
-
Last visited
Content Type
Profiles
Articles
Forums
Gallery
Downloads
Store
Posts posted by FL_Medic
-
-
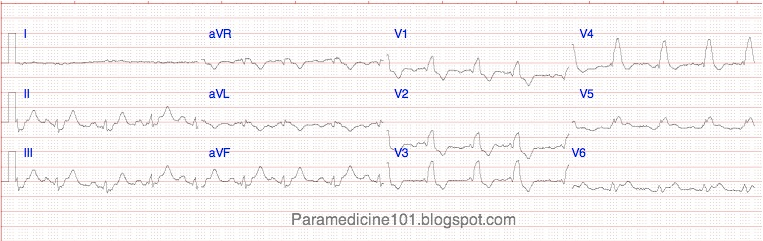
Just for fun, here ya go. I know it doesn't answer your question, but the topic made me think of it, and I figured I would share below. To answer your question, "non-specific ST-T changes" is something commonly used by the non-EP physicians out there (which is most). It is similar to an EMT telling you they got 130/palp after listening for a BP.... It isn't actually what the patient has, but it isn't necessarily a lie either. Explain to me how you could ever have a "non-specific ST-T wave change"? The change is SPECIFIC, but the etiology may be unknown.
ST-Elevation:
E - Electrolytes (hyperkalemia)
L - LBBB
E - Early repolarization (high take off)
V - Ventricular hypertrophy (LVH)
A - Aneurysm
T - Treatment (eg pericardiocentesis)
I - Injury (AMI, contusion)
O - Osborne waves (hypothermia)
N - Non-occlusive vasospasm
ST-Depression:
D - Drooping valve (MVP)
E - Enlargement of LV with strain
P - Potassium loss (hypokalemia)
R - Reciprocal ST- depression (in I/W AMI)
E - Embolism in lungs (pulmonary embolism)
S - Subendocardial ischemia
S - Subendocardial infarct
E - Encephalon hemorrhage (intracranial hemorrhage)
D - Dilated cardiomyopathy
Inverted T-waves:
I - Ischemia
N - Normality [esp. young, black]
V - Ventricular hypertrophy
E - Ectopic foci [eg calcified plaques]
R - RBBB, LBBB
T - Treatments [digoxin]
"Nonspecific" ST and T-Wave Changes
CHARLES K. FRIEDBERG M.D.1 ALBERT ZAGER M.D.1
1 From the Division of Cardiology, Department of Medicine, The Mount Sinai Hospital, New York, New York.
A study was made of 1,000 consecutive adult in-patient electrocardiograms to determine the possibility of making a more precise diagnosis than "nonspecific ST and T-wave changes." More than 50 per cent (209) of the 410 abnormal electrocardiograms (exclusive of arrhythmias) were characterized by nonspecific depression of ST segment or T wave inversion, or both.
These 209 cases comprised four groups: (1) 46 patients (22 per cent) had received digitalis, which could account for the ST-T changes; (2) 57 patients (27 per cent) had had an acute episode of cardiac pain within 5 days prior to the electrocardiogram; (3) 57 patients (27 per cent) had had no recent cardiac pain but suffered from some disease that could be regarded as a possible cause for the ST-T changes; and (4) 49 patients (24 per cent) had no apparent cause for the electrocardiographic changes. In the last group, in contrast with the others, the ST-segment depression was less than 0.5 mm. and the T-wave inversion less than 1 mm.
In patients with recent cardiac pain, as contrasted with those without such pain, the electrocardiograms were characterized by a combination of ST depression and T-wave inversion, with a depth of more than mm. of the ST depression and more than 1 mm. inversion of the T wave, by isolated T-wave inversion of more than 2 mm. and especially by more than 5 mm. in the midprecordial leads, and by an ischemic contour of the ST segment that is depressed more than mm.
There was no definite difference in the electrocardiographic findings in the patients with recent cardiac pain of less than hour and those with recent cardiac pain of more than hour when the cases with transmural infarction (Q-wave changes) were excluded. This is compatible with the concept that the electrocardiogram usually does not distinguish between subendoeardial ischemia and subendocardial necrosis. The latter differentiation would depend on multiple clinical and laboratory findings.
Differential for Non-specific ST-T wave changes
Hyperthyroid statusHyperthyroidism (Graves disease)
Postural hypotension
Hypothyroidism (myxedema)
Addison's disease (chronic adrenal ins)
Hypertension, malignant
Thyrotoxic crisis
Complete heart block
Hypertension, accelerated
Thyrotoxic heart disease
Cushing's disease/Syndrome
Early repolarization EKG syndrome
Adrenocorticoid Deficiency
Hypertension
One more source from Google:
Nonspecific ST-T wave abnormalities are very common and may be seen in any limb or precordial lead of the electrocardiogram. The changes may be seen in all of the limb and precordial leads (diffuse changes), or they may be present only in the inferior, lateral, or anterior leads.The types of abnormalities are varied and include straightening of the ST segment, ST segment depression or elevation, flattening of the T wave, or T wave inversion (figure 1). Causes of these changes include:
Electrolyte abnormalities
Post-cardiac surgical state
Anemia
Fever
Acidosis or alkalosis
Catecholamines
Drugs
Acute abdominal process
Endocrine abnormalities
Metabolic changes
Cerebrovascular accidents
Diseases such as myocarditis, pericarditis, cardiomyopathy, pulmonary emboli, infections, amyloidosis, systemic diseases, lung diseases
Abnormal T waves and ST segments may also be seen in healthy individuals, including well trained athletes.
-
NEXUS criteria do not apply to the elderly for exactly this reason. The Canadian C-Spine Rule specifically excludes patients over the age of 65, and NEXUS has not been validated in this population and therefore does not apply. They are at very high risk for fracture despite minimal mechanism of injury, have underlying bone disease such as osteoarthritis, lack much of the supporting musculature that younger patients have, and frequently perceive pain differently from younger patients. Physical exam alone in geriatric patients, for a whole variety of conditions, is notoriously unreliable.
I have had dozens of elderly patients with c-spine fractures from ground level falls. I've found several c-spine fractures on elderly folks that were days or weeks old. Even in unstable fractures from these falls, neurological symptoms have not been present in many.
This is one of those situations where you really do need to immobilize them, regardless of what your gut says. You can take the compassionate approach to c-spine with a c-collar and scoop or a c-collar and securing well to the cot, but you have to treat for this injury.
'zilla
Where's the evidence that advocates spinal immobilization? There is no evidence that shows our methods of spinal immobilization does anything to protect even a known injury to the cervical spine. I hear what you're saying, and I have read it all too. However there is more evidence showing that you will further injure a patient using our traditional methods. Of coarse, I'm not ready to sit on the stand and defend that stance until my MD is ready to accept the data. Just thought I'd play devil's advocate.
-
-
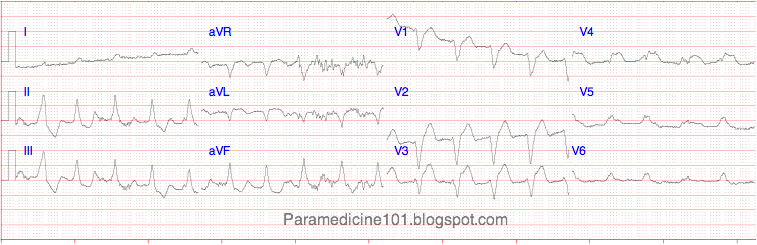
Eh, Basic question... Does the pain radiate anywhere? What does V4R show? Posterior V7,V8,V9 show any depression, Elevation? LBBB new for this PT?, ACS maybe, With Timeline, Transmural Infarct maybe, Myocarditis... Maybe. Cardiac packet labs. CPk-MB^, Troponin^, BUN/Creatine^, Potassium^, WBC^? Syncopal episodes? Febrile? Pupils equal/reactive? H/A? Tinnitus? Blurred vision? Paresthesia? Any HX of AMS in recent hours?
I disagree with FL_Medic on Paramedics interpreting 12 Leads. If you, Or your Medics have issues with 12 Leads in your area, Then maybe y'all should reevaluate your curriculum. Why would you even consider not doing a 12 Lead with a 3,4,5 lead showing ectopy? ECG Interpretation in the field is huge in our area with our Medical Directors and receiving facilities. And yes... I said diagnose and treat for the people about to jump all over that. Maybe we just have good training, And know what were doing? Don't mean to sound arrogant.
I meant for pediatric patients. If you read my blog you will see I a more than an advocate for 12-leads which are the standard of care. Pediatric patients exhibit 12-lead findings that even ER physicians don't understand.
-
12-lead ECGs are not recommended for paramedics to do... because we will see much more than there really is most of the time. Pericarditis is possible, is he sick, febrile, positional pain? Early repolarization is very likely in the young patients. They will almost always present with a degree of ST-elevation. Large QRS complexes in precordial leads indicate LVH in adults, but I think this may be benign in kids. The width of the QRS complexes is of concern. Usually depolarization is much faster the younger you are.
-
Pacing is used to try to increase heart rate.
Compressions provide a mechanical pulse.
Without a mechanical pulse, the electrical heart rate provided by pacing is of little use.
Think of reasons they are in arrest. Pacing does not ultimately cure any of them.
When you are providing chest compressions, you are pumping the blood out of the heart because the heart isn't able to do it on it's own. The pacemaker internal or external, does not pump blood. It attempts to stimulate the heart's own electrical pathways in hopes of having a mechanical reaction. Thus, the heart of a patient in cardiac arrest has gone beyond the point of pacemaker usefulness.
I have seem few try pacing in cardiac arrest, and it has never worked. I really wonder if anyone has seen it work?
I figure you can always try pacing, but chances are it is not going to circulate or get capture. Is the capture a femoral pulse or just capture on the monitor?
I have to agree with Mike. Even here in the city where I work we work the cardiac arrest for 20 minutes with a few other basic criteria but do not transport if no ROSC after calling medical control. There is more criteria to it than that but that is the basic of the protocol.
Pacing was part of the PEA/Asystole recommendations from AHA. I believe it was removed in '05.
-
What professionalism when talking over the radio.
-
This came up at work this week, and much discussion has ensued – I am hoping to get some input from the members here.
The discussion was regarding patient position while obtaining 12 lead. One staff member said that patient must be supine, as having the patient in Fowler’s position may affect axis deviation or other deviations. Another staff member said you can have the patient in Fowlers without having any change in the tracing.
When obtaining a 12-lead ECG, how important is patient positioning? If you do serial 12-leads, if the patient is in a different position during a later reading, will that affect the reading? Does anyone have evidence-based references?
I have looked through several texts I have, and have found the following:
“Although it may not be immediately obvious, the position of the patient can affect the ECG. One reason for differences between tracings obtained in various positions is that although the electrode does not move when the patient changes position, the position of the heart does move relative to the electrode. Strictly speaking, a patient should be supine when the ECG is acquired. This makes comparison of serial ECGs more meaningful. However, this is not always possible or desirable in the chest-pain patient. If the patient is not supine when the tracing is obt5ained, simply note the patient’s position on the 12-lead.”
- Phalen, T., & Aehlert, B. (2006). The 12-Lead ECG in Acute Coronary Syndromes (2nd ed., p. 50). Philadelphia: Elsevier Mosby.
“Ideally, the patient should be lying down (supine). Often, however, this is not possible. A patient with acute onset of chest pain, for example, may not feel comfortable lying down. Therfore, the Fowler’s position (sitting up) is generally used for acute patients.”
- Page, B. (2005). 12-Lead ECG for Acute and Critical Care Providers (p. 6). Upper Saddle River: Pearson Prentice Hall.
The doc and the medic involved in this discussion said that patient positioning does make a difference, but the nurse said not. However, I have spoken with another medic who also said that since the leads are only reading electrical activity, patient positioning isn’t important.
Your input is greatly appreciated.
Well the medic was right in the sense, that if you are looking to determine STEMI or not, position will have very little effect. However, it could shift the axis, only slightly. In the prehospital world, I would venture to state that Fowler's or supine are both appropriate for obtaining a 12-lead ECG. There are many other factors, that skew 12-leads, that should be of more concern.
-
I'm actually glad he used that blog post as a reference. Probably because I am favoring my own work a bit. If you read the post, I provided multiple research references. The post was more towards King LT vs. intubation for cardiac arrest. With the emphasis on continuous chest compressions, I have found that the King LT is superior [to intubation]. On the flip-side, outside of cardiac arrest, endotracheal intubation is by far a better means of controlling the airway. I wrote that particular post about a year ago, and I am sure there has been much more research provided since. A query on Pubmed may be in order. Also, I do disclaim that it is just a blog, and as I do try to only advocate evidence-based medicine, my opinion is riddled throughout.
-
I definitely agree that ventilations should be given sparingly (every 6-8 seconds which is a long time if you count it out). As for increased intrathoracic pressure, that's where the ResQPod comes in. At least, that's the Wake County EMS approach, and it seems to be working quite well!
Tom
Our system is having great results using the ResQPod, as well as Collier Co. EMS.
-
Glad everyone is alright. Also hope the patient they were going to help also got the help they needed.
Helicopters have always been dangerous and were never meant to fly. Even though they are so awesome!
Stay safe everyone.
The patient was a BLS head LAC. Only flying due to difficult egress from the island.
-
Below is the drug math tutorial from Paramedicine 101.
-
Yes, I revised that statement in my last post at the top of this page.
Thx Tom.B, I will check out the podcast.
Just wanted to stop you before you made a big mistake. Hey, it wasn't until at least my second year on the road when I learned how dangerous WPW can be. Big ups on your early motivation. Tom won't plug his own page, but I recommend you head over to his blog. Be forewarned, you might be wondering where 4 hours went, after you get done reading. Its addictive, well at least for EMS dorks like me it is.
-
1. O2
2. Normal Saline
3. Sodium Bicarb
4. Calcium
5. Lasix
6. Insulin
-
hmmm..... kinda makes me want to just cardiovert... or if fairly stable, move to amiodarone or diltiazem.
And yes..... it is 2hrs since my post above......and ya, I am still reading lol
Please don't give Cardizem!!!!
I hate to go plugging my blog again, but this specific topic was discussed there. Check it out.
Click >>>>Paramedicine101
-
I would consider cardiology my strong point but one thing I can't get my head round is electrolytes and how they effect electrical conduction; if you could cover that some point it'd be wicked
Thanks dude

I plan on giving an excellent tutorial on electrolytes and action potentials, since they are hard to figure out. Just not yet.... since this is basic and for ECG interpretation. I will start on it soon though, no worries.
Part 2
-
I have started a tutorial that will teach ECG interpretation. I started with a cardiology review, and here it is for any of you that would like a refresher.
-
http://www.medicine.nevada.edu/dept/IMNort...SKulick_001.pdf
Page 5, third point.
"Almost always located infranodal (the bundle branches), which means that the QRS duration is wide."
I do see your point and it is quite valid. I suppose you could have either.
The AHA also makes several interesting points on their website..
"This type of block [Type II second-degree AV block] most often occurs at the level of the bundle branches."
"Conducted P waves may display a normal QRS complex if the site of block is within the bundle of His, or a bundle branch block pattern if it is more distal, as in the bundle branches, which is more common."
Its moot anyhow, by my calculations the QRSd is 120ms
-
Spenac, I don't know if I advocate a 15-lead on every patient. There are indications, which can be found on a 12-lead, for 15-leads.
EMS_Cadet
Where have you read that Mobitz 2 almost always originates in the bundle branches? Mobitz 2 is commonly an infranodal block, but of the his bundle above the bundle branches. .
Click >>>THE ANSWER
-
I understand your concern, but these handicapped people live like this every day. Their mobility/sight/hearing may be impaired, but they have ways to cope. I would certainly point out to a person who may have these issues of your concern. Say a person with diarrhea, who may need to make frequent trips to the bathroom, but ambulates with a cane, refuses transport. You see the potential for falls, etc, and point out these facts to the patient and make certain their refusal is indeed an informed consent.
We have something called a "211". It is a social services referral that is coordinated with the United Way that we input into our documentation software. In situations like these, we ask the patient if they need help that doesn't require emergent treatment. We input their 211 and it is automatically sent to United Way. The patient can then seek services like home health care, non-emergent transport, etc... I recommend this to all agencies.
-
anyone else??
-
There ya go.
-
Thanks Kiwi.
-
Now Kiwi, did you miss the instructions on how to Insert Spoiler?



Job Opportunity - Lee County EMS
in General EMS Discussion
Posted
Link to Lee County website
Lee County EMS is now accepting applications to fill EMT positions. Experienced paramedics should still apply. Great pay and benefits with an aggressive EMS system in sunny SouthWest Florida.
Do not pass up this opportunity! It closes on 10/04/10